Volume 8, Issue 2 (Winter 2023)
Health in Emergencies and Disasters Quarterly 2023, 8(2): 133-144 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Dargahi A, Vosoughi Niri M, Zandian H, Poursadeqiyan M, Hamidzadeh Arbabi Y. Determinants of Noncompliance With Health Guidelines Related to COVID-19 in Ardebil, Iran Based on Network Analysis Process. Health in Emergencies and Disasters Quarterly 2023; 8 (2) :133-144
URL: http://hdq.uswr.ac.ir/article-1-348-en.html
URL: http://hdq.uswr.ac.ir/article-1-348-en.html
Abdollah Dargahi1 

 , Mehdi Vosoughi Niri2
, Mehdi Vosoughi Niri2 
 , Hamed Zandian2
, Hamed Zandian2 
 , Mohsen Poursadeqiyan3
, Mohsen Poursadeqiyan3 

 , Yousef Hamidzadeh Arbabi
, Yousef Hamidzadeh Arbabi 

 4
4


 , Mehdi Vosoughi Niri2
, Mehdi Vosoughi Niri2 
 , Hamed Zandian2
, Hamed Zandian2 
 , Mohsen Poursadeqiyan3
, Mohsen Poursadeqiyan3 

 , Yousef Hamidzadeh Arbabi
, Yousef Hamidzadeh Arbabi 

 4
4
1- Department of Environmental Health, Khalkhal University of Medical Sciences, Khalkhal, Iran.
2- Social Determinants of Health Research Center, Ardabil University of Medical Sciences, Ardabil, Iran.
3- Department of Occupational Health and Safety Engineering, School of Health, Ardabil University of Medical Sciences, Ardabil, Iran.
4- Department of Occupational Health and Safety Engineering, School of Health, Ardabil University of Medical Sciences, Ardabil, Iran. , hamidzade2015@gmail.com
2- Social Determinants of Health Research Center, Ardabil University of Medical Sciences, Ardabil, Iran.
3- Department of Occupational Health and Safety Engineering, School of Health, Ardabil University of Medical Sciences, Ardabil, Iran.
4- Department of Occupational Health and Safety Engineering, School of Health, Ardabil University of Medical Sciences, Ardabil, Iran. , hamidzade2015@gmail.com
Full-Text [PDF 592 kb]
(324 Downloads)
| Abstract (HTML) (949 Views)
Full-Text: (297 Views)
1. Introduction
The world has faced a new phenomenon that is the COVID-19 pandemic. This pandemic has changed people’s lives significantly in various aspects, such as education, business, transportation, culture, tourism, healthcare, and treatment, as well as their physical, mental, and emotional well-being [1]. The outbreak of COVID-19 has entangled the healthcare system of many countries [2]. This disease has become an international public health emergency [3, 4]. The death toll is rising so that until December 20, 2021, more than 274 million people were affected by the virus, and more than 5 million and 350 thousand individuals died [5].
In Iran, the first cases of COVID-19 were detected on February 2021 [6]. Following the doctor’s orders is one of the predictors of the successful treatment of the disease. Also, the guided use of the drugs with the healthcare specialist’s prescriptions reduces the complications and intensity of the disease [7-9]. In various studies, the prevalence of non-adherence to the prescribed drug or treatment ranges from 18% to 71%. This negligence could be the reason for a 10% increase in hospitalization and 23% in stays in nursing homes. Also, the rate of hospitalization due to not following the prescribed treatment and inadequate attention to the prescribed drug in the US reached up to 69% and imposed a $100-billion cost on this country’s healthcare system. In contrast, individuals who follow their treatment and drug achieve 20% better results [10, 11]. By determining the reasons for overlooking health protocols, oriented policies and programs, along with accurate interventions, can be used to enhance individuals’ participation and motivation to follow such protocols and improve the efficacy of previously designed programs. The results of the study by Shiloh and Peleg, and Nudelman have shown that commitment and efficacy of perceived protective behaviors have decreased gradually while the perceived anxiety from COVID-19 has increased [12]. The results of a study by Wright and Fancourt have demonstrated that the significance of many factors in predicting adaptability during pandemics is different and based on specific backgrounds [13]. Similarly, in Iran, the results of conducted studies show these differences. For instance, fear of COVID-19, controlling the perceived behavior and occupation status, the feeling of having job security, and social fear impact the protective behaviors toward COVID-19 [14, 15]. Mar’ashi has listed the following 20 factors for attendance or unattendance to protective behaviors for COVID-19: 1) information; 2) an abundance of conflicting and voluminous messages; 3) the role of the healthcare system; 4) how health recommendations are followed; 5) the role of “belief” and “attitude” (information alone is not sufficient. The information is effective in healthcare behaviors when it leads to “belief” and then an attitude); 6) believing the value of being healthy; 7) the pattern of effective healthcare beliefs (belief about the real nature of COVID-19 risks and comprehending the intensity of the problem, believing the vulnerability of oneself toward the virus, believing the efficacy of healthcare protocols, believing the value of complying to healthcare protocols as compared to the costs of catching the virus); 8) self-efficacy as an effective belief; 9) attending the principles of convincing; 10) the role of fearful messages; 11) the repetition of messages; 12) good messengers; 13) internalized social norms; 14) positive and negative reinforcement; 15) giving pattern to the society; 16) social support; 17) and ignoring negligence [16-21]. Numerous studies show that research on the effective factors of non-adherence to healthcare protocols regarding COVID-19 is either insufficient or limited to some specific aspects. However, in this study, the effective factors in not complying with COVID-19 protocols are identified and listed based on their importance. The list is provided for subjective judgment. It is hoped to arrive at more efficacious decisions regarding controlling the COVID-19 pandemic by recognizing the effective factors that encourage people not to comply with healthcare protocols.
2. Materials and Methods
This research was a descriptive-correlational study, and the study population included members of channels and groups on the WhatsApp social media platform in Ardebil City, Iran. The Morgan sampling table [22] for a 100000 population showed that 384 samples are enough for this research. A total of 366 subjects viewed the questionnaire, and 128 completed it. The mean time to complete the tool was 10 min. The inclusion criteria were being a member of WhatsApp, having proficiency in Persian, and participating in completing the questionnaire. The data collection tools were an online questionnaire created on the Porsline platform and sent to the channels and groups on WhatsApp. Regarding the effective factors in non-adherence to healthcare protocols, 67 variables were considered in the following 6 categories: individual, economic, social, cultural, media, and managerial. Considering the qualitative nature of each variable and using the 5-point Likert scale, we did not use the factor analysis method for analyzing the data and instead used multifactorial decision-making for determining the weight and priority of each variable.
One of the common methods in multifactorial decision-making is the analytical network process (ANP) that we used in this model. To implement the ANP method, we used the R software. Considering the quantitative and continuous scores of factors, we used the factorial analysis method to determine the weight of each of the 6 factors. In this regard, it is important to maintain the following notes. The kaiser-meyer-olkin (KMO) measure of sampling adequacy equaled 0.840, which is close to 1; therefore, the sample size is sufficient for conducting factorial analysis.
Also, since the significance of the Bartlett test of sphericity was smaller than 0.05, conducting factorial analysis was suitable for the data set. Additionally, the obtained variance was 70.47, indicating that 70.47% of the alterations in the data of these 6 variables are explained by a more comprehensive variable. To calculate the validity of the questionnaire, the questionnaire items were presented to a panel consisting of 6 faculty members of the research field, and their feedback was applied to the tool. Finally, 60 variables were included in the research. To calculate the tool’s reliability, we used the test-retest method in a 2-week interval at the workplace with 15 individuals. The mean scores of all items in these two phases ranged from 0.63 to 0.89. However, the Cronbach α method showed the mean score of the items in a questionnaire at 0.77 for the two phases. The questionnaire contained three subsections: introduction, demographic information, and questions regarding the effective factors of not complying with healthcare protocols regarding COVID-19. Finally, the obtained data were analyzed via descriptive statistics (simple abundance, simple percentage of abundance, Mean±SD), correlation coefficient (the Pearson correlation coefficient and the Spearman nonparametric correlation coefficient), along with the ANP method and factorial analysis via the SPSS software, version 20.
3. Results
The results regarding the demographic information of the participants are provided in Table 1.

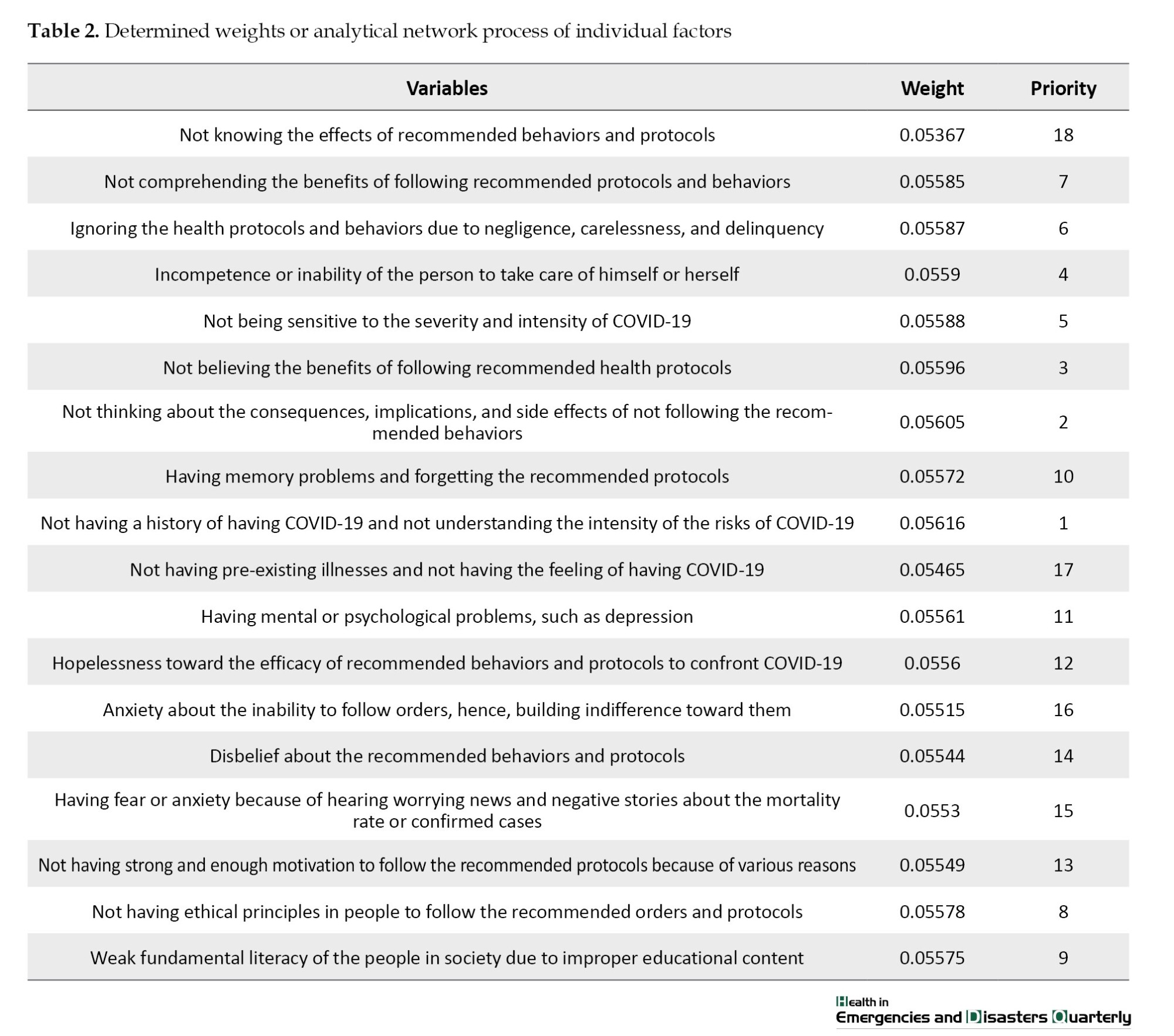
The corresponding variables, or the 6 studied variables, with their given weights and values, are provided in Tables 2 to 7.
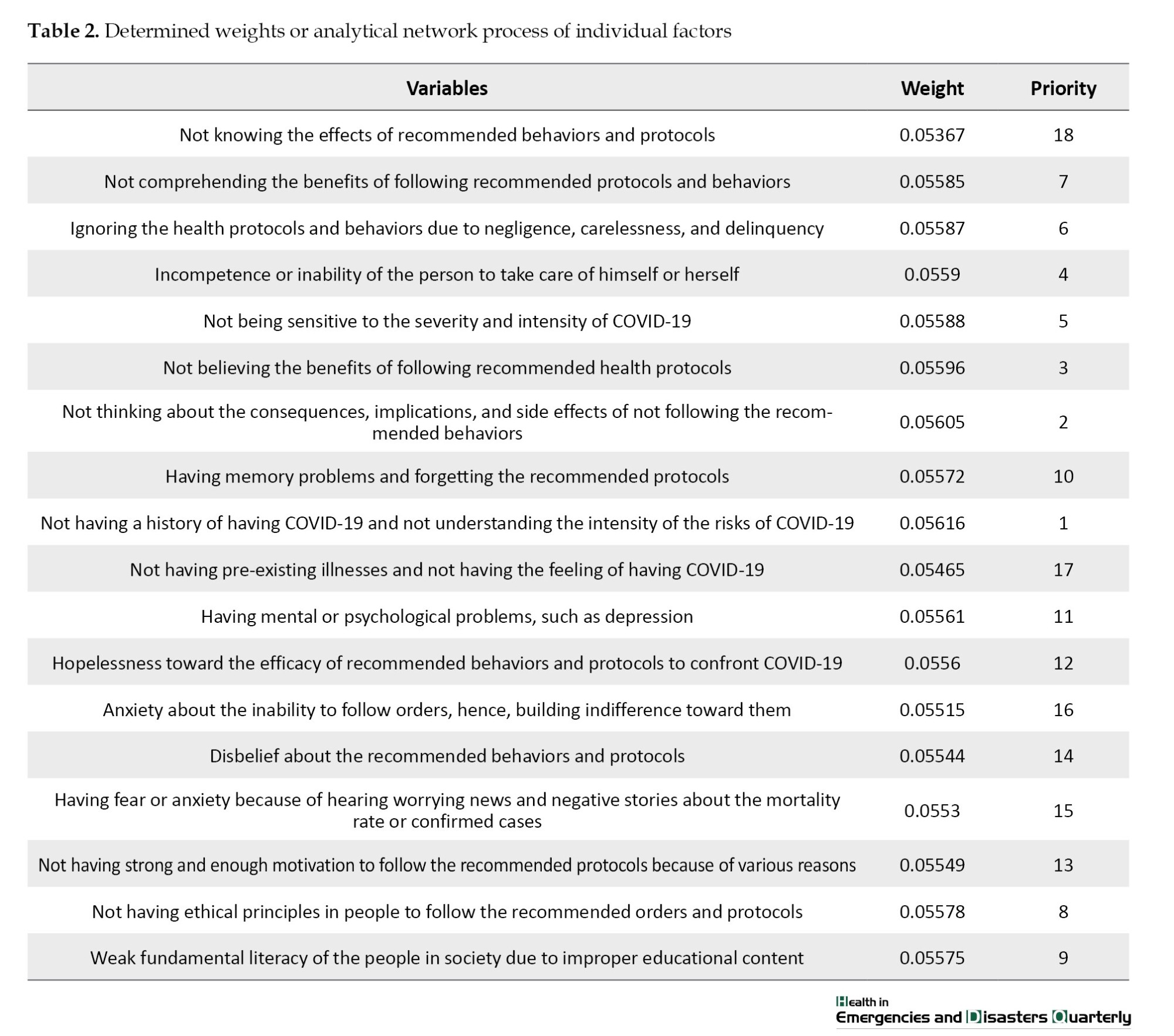
Individual factors
Eighteen out of the 60 variables were classified as individual factors. By employing the ANP method in R software, the weight of each variable was calculated, which shows the importance of the variable. In Table 2, two variables of “having no history of catching COVID-19 and not understanding the intensity of the risk of COVID-19” and “not thinking about the consequences, implications, and side-effects of not following the recommended protocols and behaviors” were the most important individual factors. Meanwhile, two individual factors of “having no pre-existing illness and having the feeling of not catching COVID-19” and “anxiety about self-capabilities for following the recommended protocols and ignoring them” were among the least important variables.
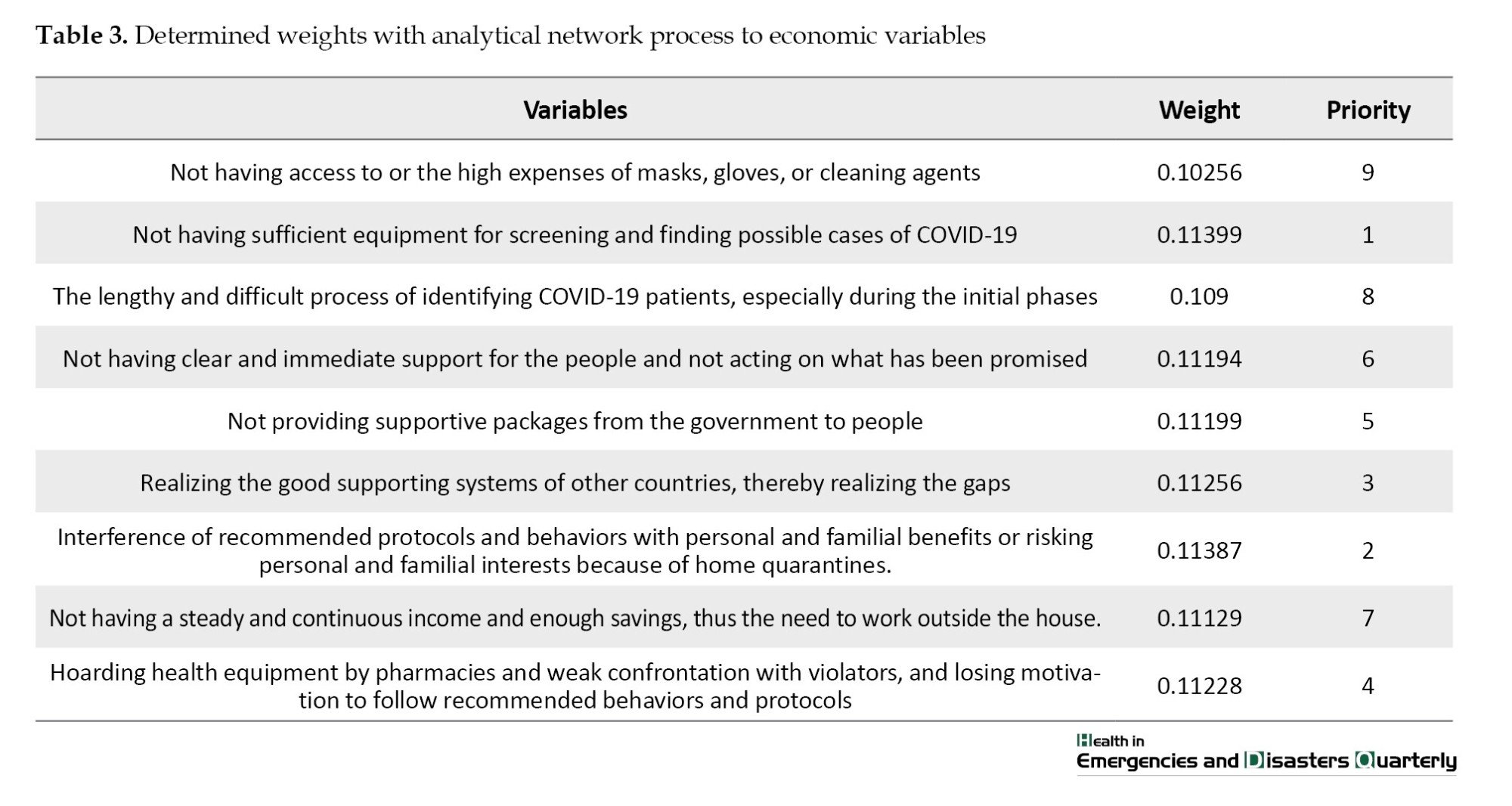
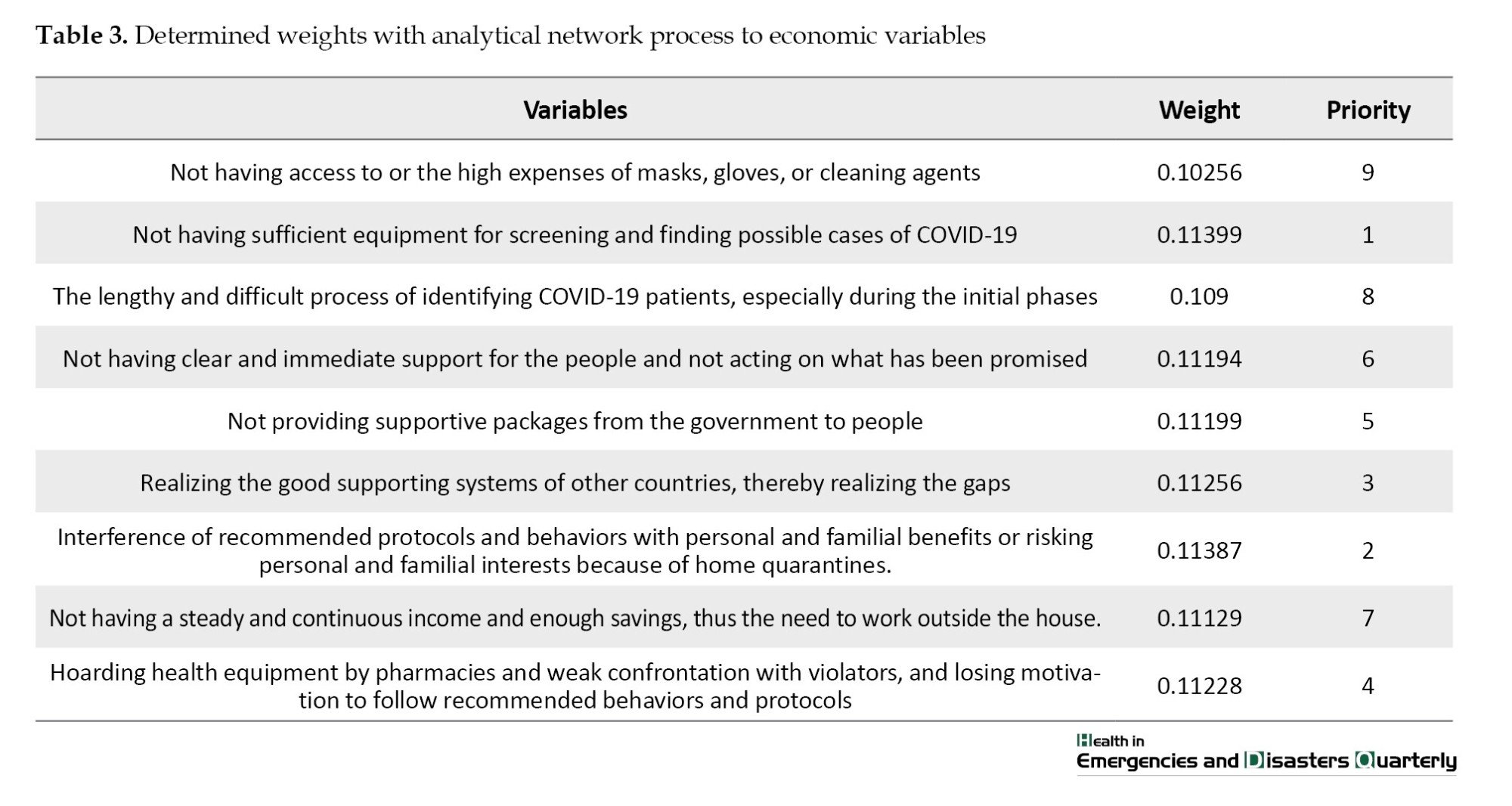
Economic factors
Nine out of 60 studied variables were classified under the economic factor and then calculated via the ANP method. The results are provided in Table 3. Considering this Table, two variables of “not having enough equipment to conduct screening, examining, and finding possible cases of COVID-19” and “risking personal and familial benefits by following home quarantines” were the most important economic factors.
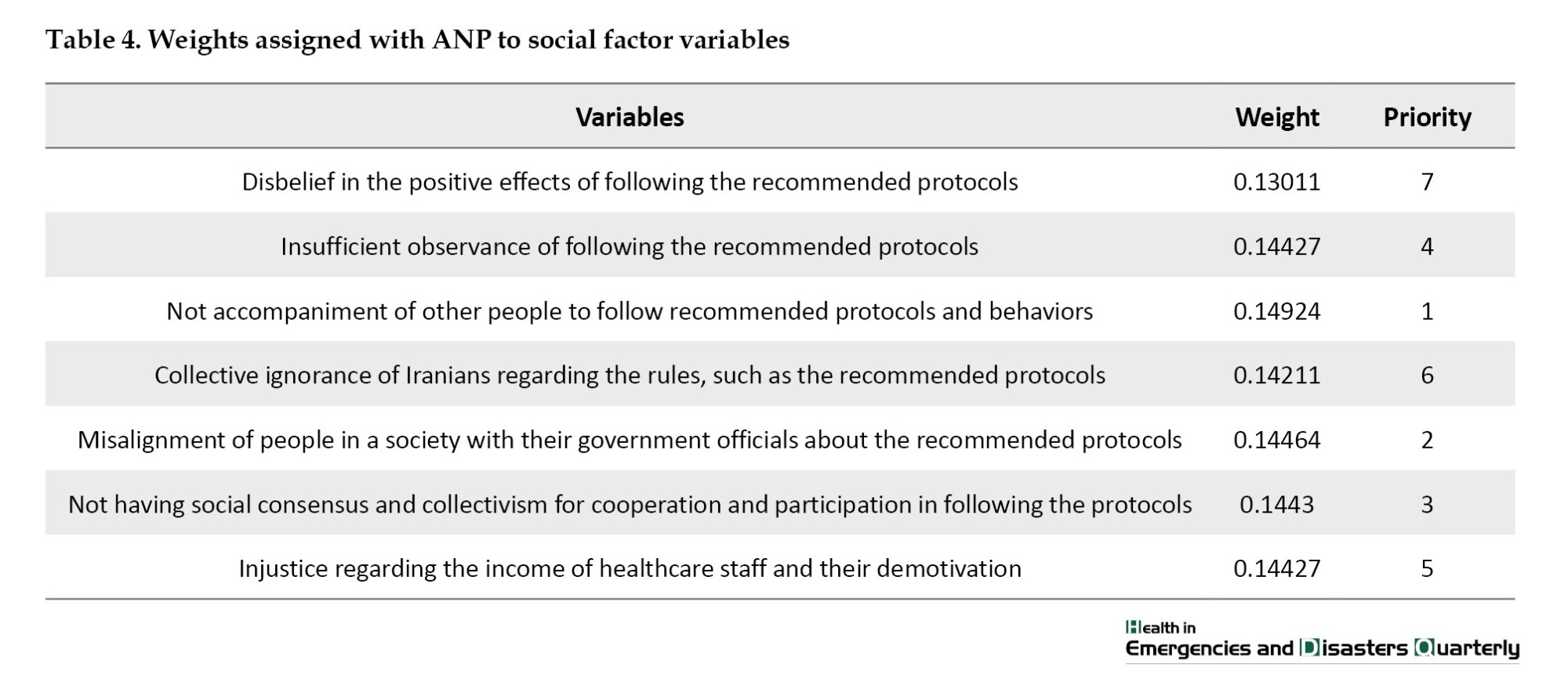
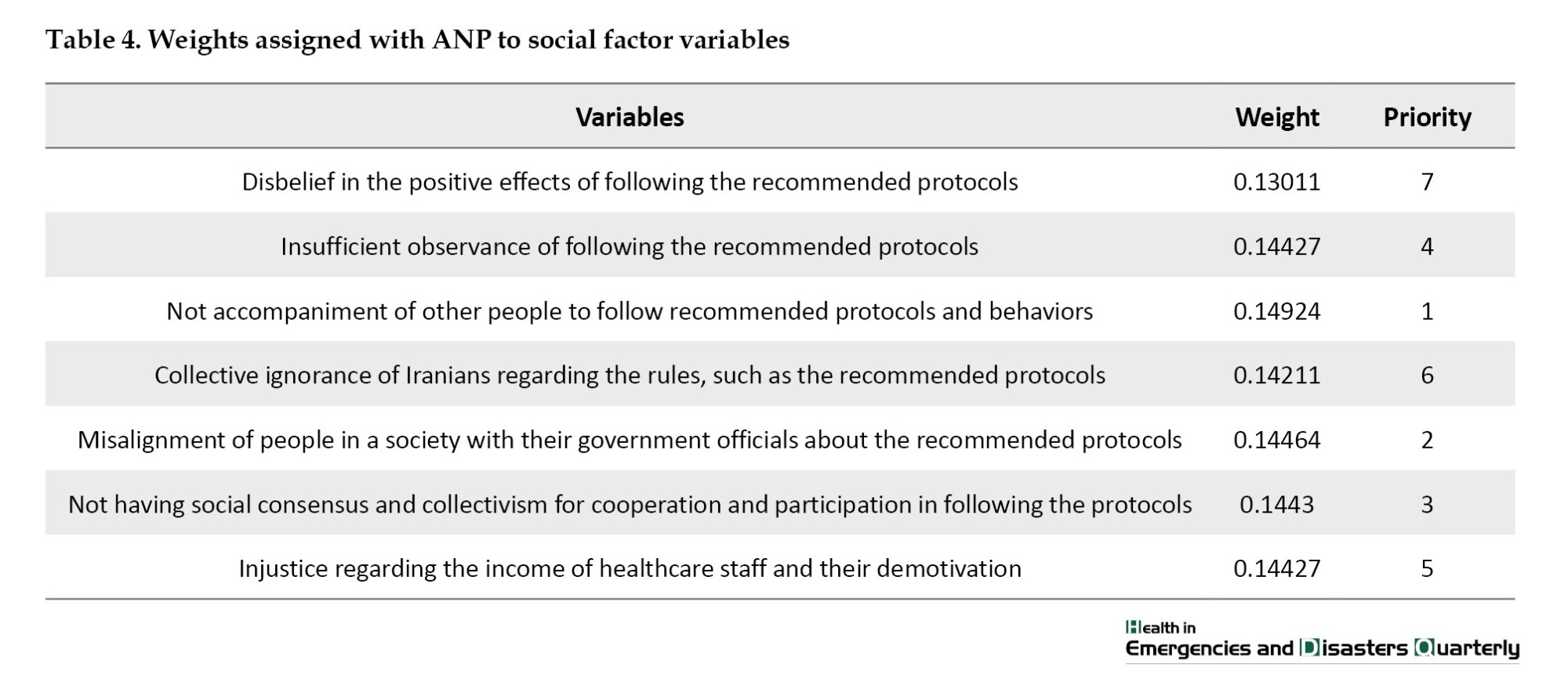
Social factors
Seven out of 60 studied variables were classified under social factors and then calculated via the ANP method. The results are provided in Table 4. In this Table, two variables of “not an accompaniment of others to follow recommended protocols” and “misalignment of people in a society with their government officials about the recommended protocols” were the most important factors. In contrast, “disbelief about the positive effects of following the protocols” and “collective avoidance of people from the rules, such as the recommended protocols”, were the least important variables of social factor.
Cultural factors
Three out of 60 studied variables were classified in terms of cultural factors and then calculated via the ANP method. The results are provided in Table 5. In this Table, the “facing cultural-economic deprivation because of following the recommended protocols” and “families’ expectations to meet other relatives, regardless of the COVID-19 situation” variables were the most important variables of cultural factors.

Media factors
Six out of 60 studied variables were classified in terms of media factors via ANP and listed in Table 6. According to this Table, the two variables of “false news, gossip and conflict in people” and “sending very simple, ambiguous or impractical news regarding COVID-19” were the most important media factors.

Managerial factors
Seventeen out of 60 studied variables were classified as managerial factors via the ANP method and are listed in Table 7. According to this Table, “the effects of sanctions, increasing prices, and the difficulty of life,” “not controlling the roads and not limiting the travels from the beginning of COVID-19 pandemic,” and “the lack of rigid deterrent rules, such as heavy fines and imprisonment” were the most important variables of managerial factors.

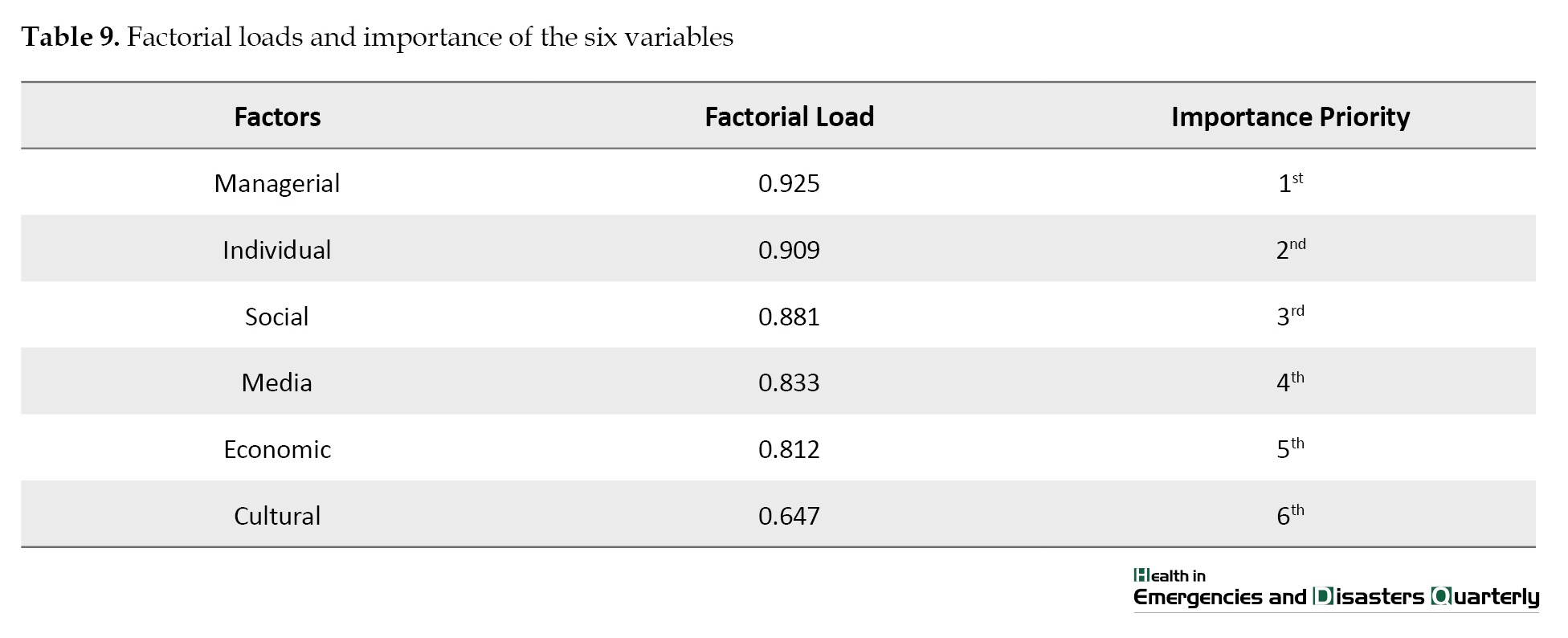
The importance of each of 6 variables
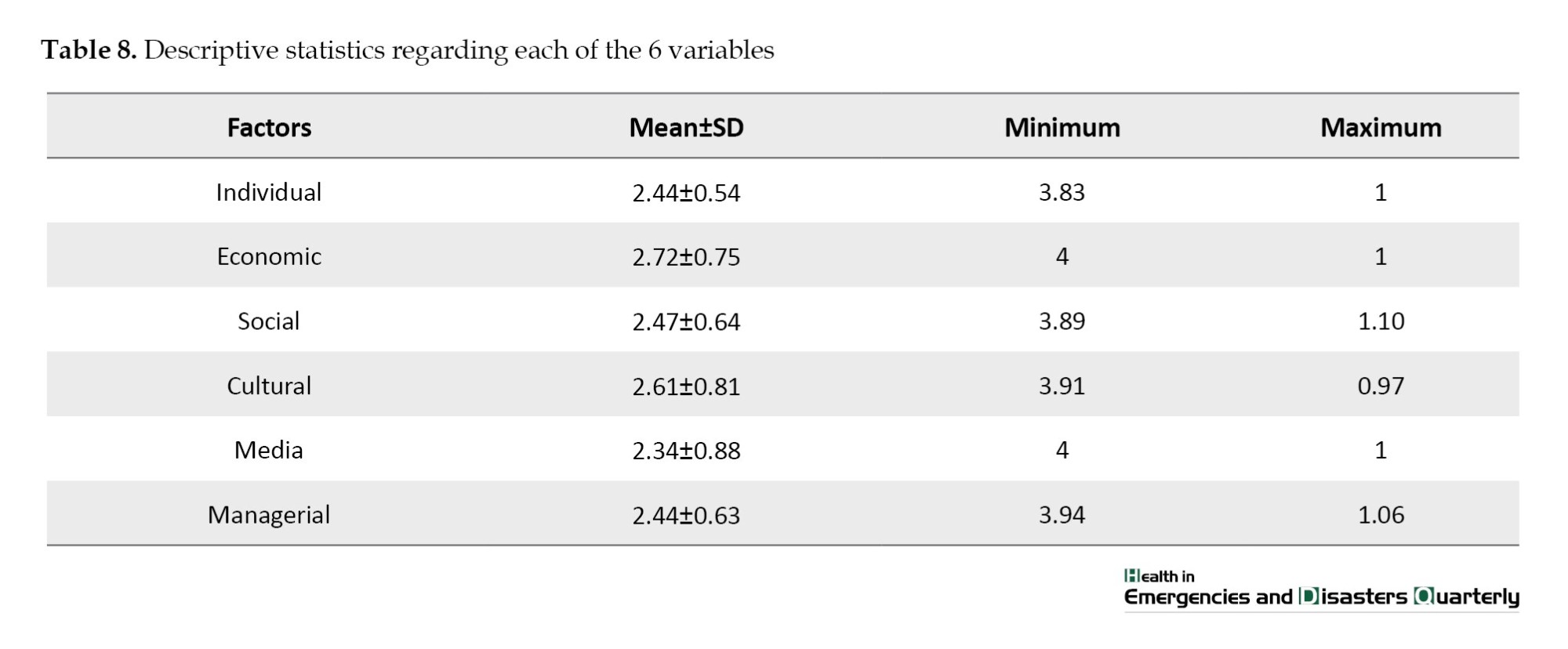
After identifying the significance of each variable in the 6 categories of factors, the importance of each factor was investigated. To better understand the status of the scores, we used descriptive statistics, such as Mean±SD, minimum and maximum. These data are provided in Table 8.
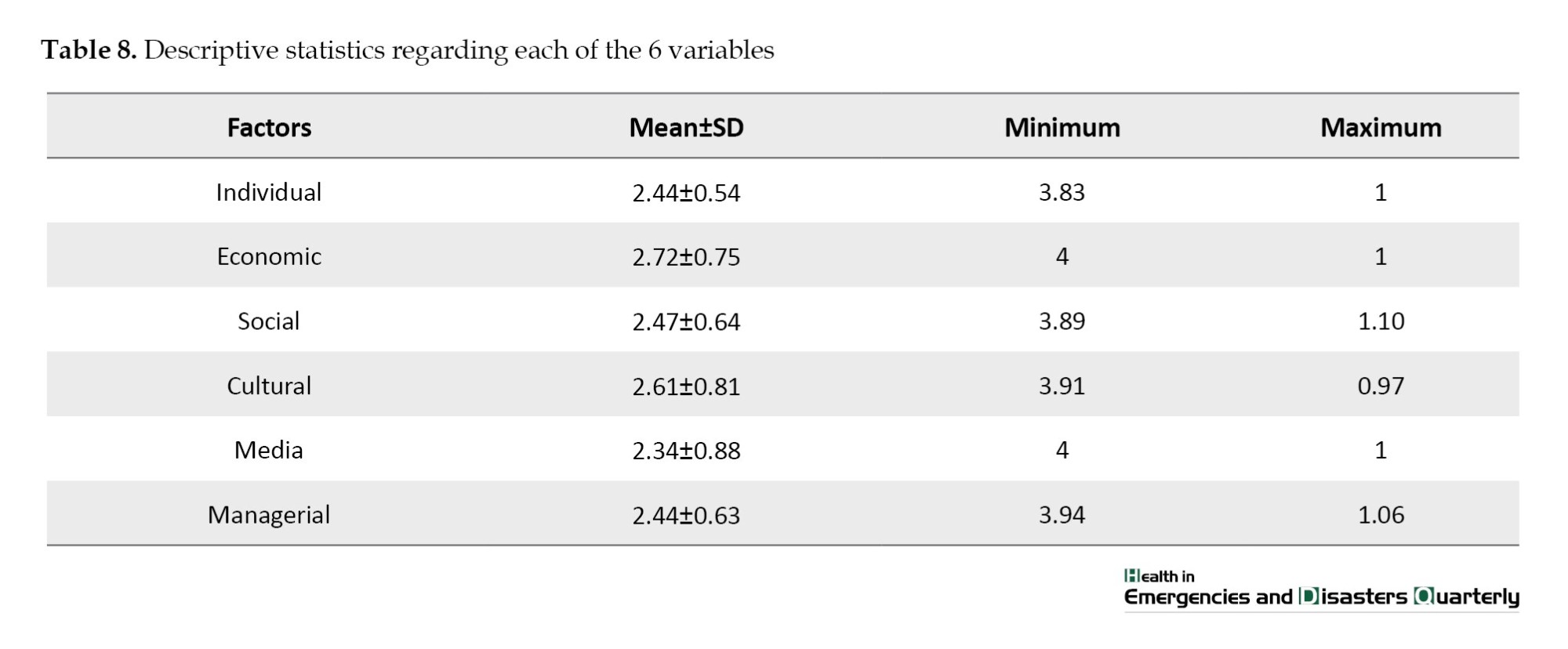
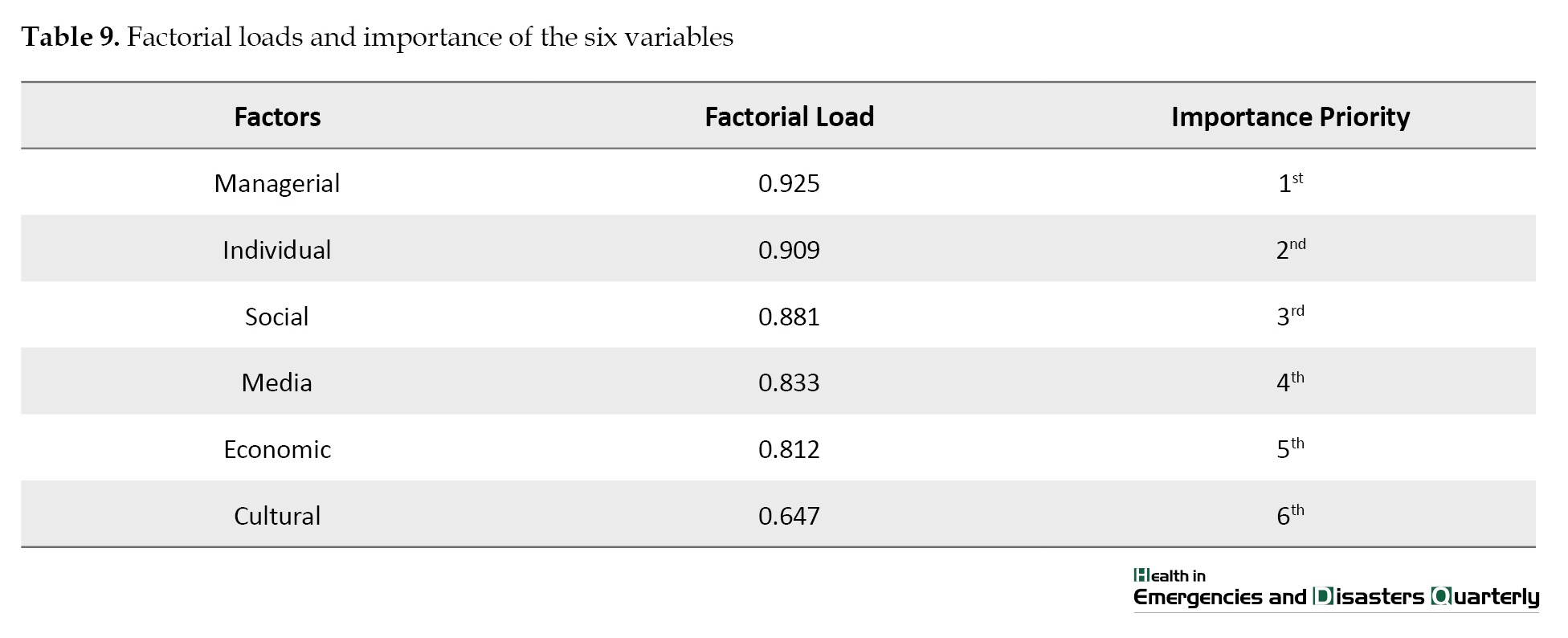
By performing factorial analysis on the data, the factorial load of each of the six factors, which shows their importance, was calculated and provided in Table 9. According to the factorial loads, managerial, individual, social, media, economic, and cultural were the most important factors that make people not follow the health protocols provided by the national center for confronting COVID-19.
To investigate the relationship between age and scores of each of the variables that are effective in following the protocols, we used the Pearson correlation coefficient. The variable of age, with a negative correlation coefficient, had only a significant relationship with cultural and media factors (Sig.=0.031, R=-0.191) and (R=-0.312, Sig.=0.000). Accordingly, with increasing age, the effect of cultural and media factors in following protocols reduces.
Relationship between discrete demographic variables and effective factors in following the protocols
The studied discrete demographic variables included gender, marital status, number of children, occupation type, education level, place of residence, source of information, history of having COVID-19, and history of using drugs. To analyze the correlation of each of these demographic variables with the 6 studied variables, at first, we categorized them based on their scores into 4 classes of low, medium, high, and very high via the Chi-square method. The gender variable showed a significant relationship (P=0.030) with the media factor at a 95% confidence interval. Accordingly, male participants, compared to female participants, used media more. The variable of marital status was significantly related to individual, cultural, and media factors at a 95% confidence interval (P=0.008, P=0.021, and P=0.005).
Accordingly, married participants, compared to single participants, considered individual, cultural and media variables more involved in following the protocols. The education level had a significant relationship with personal, economic, and cultural factors at a 95% interval (P =0.048, P=0.0016, and P=0.0009). Accordingly, participants with university education considered individual, economic, and cultural factors effective in following the health protocols. The place of residence had a significant relationship with cultural and managerial factors at a 95% confidence interval (P=0.000, P=0.006). People who live in urban areas consider cultural and managerial factors more effective in following the health protocols compared to residents of rural areas. The type of occupation had a significant relationship with the individual, economic, and social factors (P=0.012, P=0.0006, and P=0.001) at a 95% confidence interval. Employees considered individual, economic, and social factors more effective in following health protocols than other occupations. History of having COVID-19 had a significant relationship with social and media factors (P=0.0001 and P=0.016) at a 95% confidence interval. Also, the source of information had significant relationships with individual and managerial factors (P=0.013 and P=0.046) at a 95% confidence interval. Participants who used the internet and government television considered individual and managerial factors more effective in following health protocols.
4. Discussion
According to our study, managerial, individual, social, media, economic, and cultural factors are the most important factors in this order that make people not follow health protocols set by the national center for confronting this disease. The most important factor in this regard was the managerial factor or the inefficiency of managers. In modern terms, management refers to behaviors that people demonstrate according to their status in an organization. The behaviors should be based on theories and values they believe in and follow individually. These behaviors might be practical and can be performed, or they might be based on thoughts or metaphysical aspects without practical aspects [23, 24]. The proper executive management of a country considers this virus an enemy and, in confronting this pandemic, emphasizes the tools and weapons for fighting with the enemy. Also, the managers highlight the capabilities of the country in fighting the disease, along with giving hope and strengthening the relationship between people and the government [25]. Also, for an efficient management team to fight a crisis such as the COVID-19 pandemic, passing mandatory laws along with social and economic support such as paying subsidies and compensations to the vulnerable strata of the societies, supervising the enactment of the law and processes of confronting those who do not abide with the laws and health protocols are necessary [26]. Wright and Fancourt demonstrated that individual characteristics are more important when behaviors are more limited [13]. Among individual factors, various variables are effective in following the protocols, of which not understanding the risk of the virus because of lacking a history of COVID-19, overlooking the implications and consequences of ignoring recommended protocols, and disbelief about following the protocols were the most important ones. This finding is in line with the results of Mar’ashi, Lee, et al. and Oberli et al. [16, 27, 28]. In the present study, one of the beliefs was the feeling of not having COVID-19. In other words, the thought that the risks always apply to others and that we are immune to threats seems to be the main reason behind ignoring recommended protocols and the major cause of many confirmed cases. Additionally, a group of individuals, especially the elderly, believe that everyone’s life is determined and that there is no way to change it. People who live in deprived and rural areas around cities cannot think about changing their lifestyle or their surroundings. Therefore, they not only do not fight COVID-19 but also are indifferent to the mortality rate of this disease so that they can free themselves from their miserable lives, per se. In other words, subjective evaluation of the self from the quality and results of their behaviors depends on evaluations, expectations, and mental norms. Also, people’s behaviors depend on two factors of motivation and the ability to control the behaviors based on subjective assessment of the people (controlling the perceived behavior). In case of enough real control over behaviors and sufficient opportunities, the individual has enough willpower to perform a behavior. Similarly, Rajpura and Nayak (2014) have shown that preceding the illness, positive thoughts regarding the treatment of blood pressure are accompanied by the following treatment [29].
Perception, on the one hand, creates beliefs, and on the other hand, it is made via clear and correct information. However, information alone is not enough. It can help increase healthcare behaviors when it is turned into a belief and then an attitude. Accordingly, information, beliefs, and attitudes are the main essence of motivating people to perform healthy behaviors [30, 31]. The third and fourth factors in following the protocols were social and cultural. These findings agree with Rajjpura and Nayak, Mousavi et al., Siabani, and Mohammadi et al. [29, 30, 32, 33].
Perception of the illness in cultural and socio-economic situations can impact the following differently. For instance, Mousavi et al. have shown in their study that following treatment depends on familial and social support becomes a challenge for the person and results in their ignorance toward healthy behaviors [30]. It seems that culture sets the norms and limits of content approaches and managerial processes, thereby affecting the following protocols via acceptance or unacceptance of factors. The fifth result was regarding media. This result is in line with Wright and Fancourt and Ahmidian and Haghighatian. According to their study, cultural factors and providing information can predict responsive policies [13, 17]. In analyzing these findings, we can argue that all sorts of news are presented via media; media literacy makes viewers choose what to watch and pay attention to which news. One of the reasons for incorrect perceptions is the sending of improper messages, advertisements, and information by several media platforms. Ineffective advertisement and information provision result in the ignorance of a group of people toward COVID-19, thereby not welcoming advertising and information regarding this disease.
In addition, populistic and not scientific information provision about COVID-19 and also delivery of various opinions and scientific and not-scientific hypotheses with contradictions by media and nonexperts results in the eradication of people’s sensitivity toward COVID-19. Also, the dishonesty of government officials and delivering contradictory news by the media made a group of people cynical about the government and mass media platforms, resulting in society’s disbelief. The results of Wright and Fancourt show that an increase in trust in the government effectively confronts the pandemic [13]. Therefore, honest talks by government officials and their timely reflections and reactions by the media can be effective in people’s following health protocols. In addition, people should obtain information via proper and scientific sources regarding COVID-19. However, one of the reasons for not following health protocols during the COVID-19 pandemic might be paying attention to improper and untrustworthy media sources.
Regarding economic factors, two variables of “not having sufficient equipment for examining, screening and finding possible cases of COVID-19” and “interference of recommended protocols with individual and familial interests”, were the most important reasons for not following the health protocols. These findings are in line with the results of Gholamaline et al., Ghiasvanad, and Alizadeh. They have demonstrated that in following drug treatments, various factors such as demographic, social, and economic variables, and factors regarding the healthcare system along with factors regarding the patient are effective [18]. Ghiasvand and Taghizadeh have found occupation and people’s income status effective in following preventive behaviors, along with perceived behavior controls [15]. In analyzing these results, it can be maintained that fighting the COVID-19 pandemic is a sociocultural and economic fight while it is related to the healthcare system. Therefore, controlling this matter requires considering all impacting aspects and all social groups to plan, implement, and evaluate programs for people to follow health protocols and break the chain of prevalence.
Also, in the present study, men used media platforms more than women and married people compared to single ones considered individual, cultural, and media factors effective in following protocols. In addition, people with a university education considered individual, economic, and cultural factors effective in following the protocols. Urban citizens considered cultural and managerial factors effective in following protocols more than rural citizens. Employees found individual, economic, and social factors effective in following the protocols more than people with other types of occupations. These findings are in line with the results of Kharamin et al. Their study shows that women more than men, urban citizens more than rural citizens, married compared to single individuals, educated more than illiterate or less educated individuals, personal characteristics, and so on were effective in following health protocols [34-36]. The benefits of the present study were that almost all influential aspects of ignoring the protocols were gathered in one place and analyzed collectively, and with the use of modern statistical methods, an approach similar yet better than systematic review and thoroughly scientific was made. In addition, the order and importance of each factor that affects following the protocols were obtained.
5. Conclusion
The results of the present study showed that managerial, individual, social, media, economic, and cultural factors affect following the health protocols, and if these factors are not considered by the managers, controlling the pandemic would become harder and impose heavy human, economic, and social costs on the country. Considering the importance of controlling COVID-19 in improving the country’s health and preventing the prevalence of this disease and its implications, managers must consider affective factors in not following the protocols for designing effective programs and interventions. Therefore, by considering the identified factors and designing models based on the factors mentioned above, managers, doctors, and experts should help enhance the following protocols to reduce the negative individual, social, and economic implications.
Study limitations
Some limitations of this study were not participation and limited reception of members of the WhatsApp social media platform members, limited participation of rural citizens, the self-reporting nature of the questionnaire, and the cross-sectional nature of the study. When interpreting the findings of this study, these limitations should be considered. Finally, since the questionnaires were filled out online, it could be possible that the answers are limited to social media platforms. Therefore, the results cannot be generalized to the whole country.
Ethical Considerations
Compliance with ethical guidelines
This study received the following Code of ethics IRARUMS.REC.1399.194. The authors of this study express their gratitude toward members of the faculty and all participants who helped complete and approve the questionnaires and this study.
Funding
School of Health, Ardabil University of Medical Sciences funded this study.
Authors' contributions
The authors equally contributed to this work.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors would like to thank all the professors and university officials of Ardabil University of Medical Sciences, the staff and student of Ardabil University of Medical Sciences, and all the person who participated in the study and helped us in carrying out this research.
References
The world has faced a new phenomenon that is the COVID-19 pandemic. This pandemic has changed people’s lives significantly in various aspects, such as education, business, transportation, culture, tourism, healthcare, and treatment, as well as their physical, mental, and emotional well-being [1]. The outbreak of COVID-19 has entangled the healthcare system of many countries [2]. This disease has become an international public health emergency [3, 4]. The death toll is rising so that until December 20, 2021, more than 274 million people were affected by the virus, and more than 5 million and 350 thousand individuals died [5].
In Iran, the first cases of COVID-19 were detected on February 2021 [6]. Following the doctor’s orders is one of the predictors of the successful treatment of the disease. Also, the guided use of the drugs with the healthcare specialist’s prescriptions reduces the complications and intensity of the disease [7-9]. In various studies, the prevalence of non-adherence to the prescribed drug or treatment ranges from 18% to 71%. This negligence could be the reason for a 10% increase in hospitalization and 23% in stays in nursing homes. Also, the rate of hospitalization due to not following the prescribed treatment and inadequate attention to the prescribed drug in the US reached up to 69% and imposed a $100-billion cost on this country’s healthcare system. In contrast, individuals who follow their treatment and drug achieve 20% better results [10, 11]. By determining the reasons for overlooking health protocols, oriented policies and programs, along with accurate interventions, can be used to enhance individuals’ participation and motivation to follow such protocols and improve the efficacy of previously designed programs. The results of the study by Shiloh and Peleg, and Nudelman have shown that commitment and efficacy of perceived protective behaviors have decreased gradually while the perceived anxiety from COVID-19 has increased [12]. The results of a study by Wright and Fancourt have demonstrated that the significance of many factors in predicting adaptability during pandemics is different and based on specific backgrounds [13]. Similarly, in Iran, the results of conducted studies show these differences. For instance, fear of COVID-19, controlling the perceived behavior and occupation status, the feeling of having job security, and social fear impact the protective behaviors toward COVID-19 [14, 15]. Mar’ashi has listed the following 20 factors for attendance or unattendance to protective behaviors for COVID-19: 1) information; 2) an abundance of conflicting and voluminous messages; 3) the role of the healthcare system; 4) how health recommendations are followed; 5) the role of “belief” and “attitude” (information alone is not sufficient. The information is effective in healthcare behaviors when it leads to “belief” and then an attitude); 6) believing the value of being healthy; 7) the pattern of effective healthcare beliefs (belief about the real nature of COVID-19 risks and comprehending the intensity of the problem, believing the vulnerability of oneself toward the virus, believing the efficacy of healthcare protocols, believing the value of complying to healthcare protocols as compared to the costs of catching the virus); 8) self-efficacy as an effective belief; 9) attending the principles of convincing; 10) the role of fearful messages; 11) the repetition of messages; 12) good messengers; 13) internalized social norms; 14) positive and negative reinforcement; 15) giving pattern to the society; 16) social support; 17) and ignoring negligence [16-21]. Numerous studies show that research on the effective factors of non-adherence to healthcare protocols regarding COVID-19 is either insufficient or limited to some specific aspects. However, in this study, the effective factors in not complying with COVID-19 protocols are identified and listed based on their importance. The list is provided for subjective judgment. It is hoped to arrive at more efficacious decisions regarding controlling the COVID-19 pandemic by recognizing the effective factors that encourage people not to comply with healthcare protocols.
2. Materials and Methods
This research was a descriptive-correlational study, and the study population included members of channels and groups on the WhatsApp social media platform in Ardebil City, Iran. The Morgan sampling table [22] for a 100000 population showed that 384 samples are enough for this research. A total of 366 subjects viewed the questionnaire, and 128 completed it. The mean time to complete the tool was 10 min. The inclusion criteria were being a member of WhatsApp, having proficiency in Persian, and participating in completing the questionnaire. The data collection tools were an online questionnaire created on the Porsline platform and sent to the channels and groups on WhatsApp. Regarding the effective factors in non-adherence to healthcare protocols, 67 variables were considered in the following 6 categories: individual, economic, social, cultural, media, and managerial. Considering the qualitative nature of each variable and using the 5-point Likert scale, we did not use the factor analysis method for analyzing the data and instead used multifactorial decision-making for determining the weight and priority of each variable.
One of the common methods in multifactorial decision-making is the analytical network process (ANP) that we used in this model. To implement the ANP method, we used the R software. Considering the quantitative and continuous scores of factors, we used the factorial analysis method to determine the weight of each of the 6 factors. In this regard, it is important to maintain the following notes. The kaiser-meyer-olkin (KMO) measure of sampling adequacy equaled 0.840, which is close to 1; therefore, the sample size is sufficient for conducting factorial analysis.
Also, since the significance of the Bartlett test of sphericity was smaller than 0.05, conducting factorial analysis was suitable for the data set. Additionally, the obtained variance was 70.47, indicating that 70.47% of the alterations in the data of these 6 variables are explained by a more comprehensive variable. To calculate the validity of the questionnaire, the questionnaire items were presented to a panel consisting of 6 faculty members of the research field, and their feedback was applied to the tool. Finally, 60 variables were included in the research. To calculate the tool’s reliability, we used the test-retest method in a 2-week interval at the workplace with 15 individuals. The mean scores of all items in these two phases ranged from 0.63 to 0.89. However, the Cronbach α method showed the mean score of the items in a questionnaire at 0.77 for the two phases. The questionnaire contained three subsections: introduction, demographic information, and questions regarding the effective factors of not complying with healthcare protocols regarding COVID-19. Finally, the obtained data were analyzed via descriptive statistics (simple abundance, simple percentage of abundance, Mean±SD), correlation coefficient (the Pearson correlation coefficient and the Spearman nonparametric correlation coefficient), along with the ANP method and factorial analysis via the SPSS software, version 20.
3. Results
The results regarding the demographic information of the participants are provided in Table 1.

The corresponding variables, or the 6 studied variables, with their given weights and values, are provided in Tables 2 to 7.
Individual factors
Eighteen out of the 60 variables were classified as individual factors. By employing the ANP method in R software, the weight of each variable was calculated, which shows the importance of the variable. In Table 2, two variables of “having no history of catching COVID-19 and not understanding the intensity of the risk of COVID-19” and “not thinking about the consequences, implications, and side-effects of not following the recommended protocols and behaviors” were the most important individual factors. Meanwhile, two individual factors of “having no pre-existing illness and having the feeling of not catching COVID-19” and “anxiety about self-capabilities for following the recommended protocols and ignoring them” were among the least important variables.
Economic factors
Nine out of 60 studied variables were classified under the economic factor and then calculated via the ANP method. The results are provided in Table 3. Considering this Table, two variables of “not having enough equipment to conduct screening, examining, and finding possible cases of COVID-19” and “risking personal and familial benefits by following home quarantines” were the most important economic factors.
Social factors
Seven out of 60 studied variables were classified under social factors and then calculated via the ANP method. The results are provided in Table 4. In this Table, two variables of “not an accompaniment of others to follow recommended protocols” and “misalignment of people in a society with their government officials about the recommended protocols” were the most important factors. In contrast, “disbelief about the positive effects of following the protocols” and “collective avoidance of people from the rules, such as the recommended protocols”, were the least important variables of social factor.
Cultural factors
Three out of 60 studied variables were classified in terms of cultural factors and then calculated via the ANP method. The results are provided in Table 5. In this Table, the “facing cultural-economic deprivation because of following the recommended protocols” and “families’ expectations to meet other relatives, regardless of the COVID-19 situation” variables were the most important variables of cultural factors.

Media factors
Six out of 60 studied variables were classified in terms of media factors via ANP and listed in Table 6. According to this Table, the two variables of “false news, gossip and conflict in people” and “sending very simple, ambiguous or impractical news regarding COVID-19” were the most important media factors.

Managerial factors
Seventeen out of 60 studied variables were classified as managerial factors via the ANP method and are listed in Table 7. According to this Table, “the effects of sanctions, increasing prices, and the difficulty of life,” “not controlling the roads and not limiting the travels from the beginning of COVID-19 pandemic,” and “the lack of rigid deterrent rules, such as heavy fines and imprisonment” were the most important variables of managerial factors.

The importance of each of 6 variables
After identifying the significance of each variable in the 6 categories of factors, the importance of each factor was investigated. To better understand the status of the scores, we used descriptive statistics, such as Mean±SD, minimum and maximum. These data are provided in Table 8.
By performing factorial analysis on the data, the factorial load of each of the six factors, which shows their importance, was calculated and provided in Table 9. According to the factorial loads, managerial, individual, social, media, economic, and cultural were the most important factors that make people not follow the health protocols provided by the national center for confronting COVID-19.
To investigate the relationship between age and scores of each of the variables that are effective in following the protocols, we used the Pearson correlation coefficient. The variable of age, with a negative correlation coefficient, had only a significant relationship with cultural and media factors (Sig.=0.031, R=-0.191) and (R=-0.312, Sig.=0.000). Accordingly, with increasing age, the effect of cultural and media factors in following protocols reduces.
Relationship between discrete demographic variables and effective factors in following the protocols
The studied discrete demographic variables included gender, marital status, number of children, occupation type, education level, place of residence, source of information, history of having COVID-19, and history of using drugs. To analyze the correlation of each of these demographic variables with the 6 studied variables, at first, we categorized them based on their scores into 4 classes of low, medium, high, and very high via the Chi-square method. The gender variable showed a significant relationship (P=0.030) with the media factor at a 95% confidence interval. Accordingly, male participants, compared to female participants, used media more. The variable of marital status was significantly related to individual, cultural, and media factors at a 95% confidence interval (P=0.008, P=0.021, and P=0.005).
Accordingly, married participants, compared to single participants, considered individual, cultural and media variables more involved in following the protocols. The education level had a significant relationship with personal, economic, and cultural factors at a 95% interval (P =0.048, P=0.0016, and P=0.0009). Accordingly, participants with university education considered individual, economic, and cultural factors effective in following the health protocols. The place of residence had a significant relationship with cultural and managerial factors at a 95% confidence interval (P=0.000, P=0.006). People who live in urban areas consider cultural and managerial factors more effective in following the health protocols compared to residents of rural areas. The type of occupation had a significant relationship with the individual, economic, and social factors (P=0.012, P=0.0006, and P=0.001) at a 95% confidence interval. Employees considered individual, economic, and social factors more effective in following health protocols than other occupations. History of having COVID-19 had a significant relationship with social and media factors (P=0.0001 and P=0.016) at a 95% confidence interval. Also, the source of information had significant relationships with individual and managerial factors (P=0.013 and P=0.046) at a 95% confidence interval. Participants who used the internet and government television considered individual and managerial factors more effective in following health protocols.
4. Discussion
According to our study, managerial, individual, social, media, economic, and cultural factors are the most important factors in this order that make people not follow health protocols set by the national center for confronting this disease. The most important factor in this regard was the managerial factor or the inefficiency of managers. In modern terms, management refers to behaviors that people demonstrate according to their status in an organization. The behaviors should be based on theories and values they believe in and follow individually. These behaviors might be practical and can be performed, or they might be based on thoughts or metaphysical aspects without practical aspects [23, 24]. The proper executive management of a country considers this virus an enemy and, in confronting this pandemic, emphasizes the tools and weapons for fighting with the enemy. Also, the managers highlight the capabilities of the country in fighting the disease, along with giving hope and strengthening the relationship between people and the government [25]. Also, for an efficient management team to fight a crisis such as the COVID-19 pandemic, passing mandatory laws along with social and economic support such as paying subsidies and compensations to the vulnerable strata of the societies, supervising the enactment of the law and processes of confronting those who do not abide with the laws and health protocols are necessary [26]. Wright and Fancourt demonstrated that individual characteristics are more important when behaviors are more limited [13]. Among individual factors, various variables are effective in following the protocols, of which not understanding the risk of the virus because of lacking a history of COVID-19, overlooking the implications and consequences of ignoring recommended protocols, and disbelief about following the protocols were the most important ones. This finding is in line with the results of Mar’ashi, Lee, et al. and Oberli et al. [16, 27, 28]. In the present study, one of the beliefs was the feeling of not having COVID-19. In other words, the thought that the risks always apply to others and that we are immune to threats seems to be the main reason behind ignoring recommended protocols and the major cause of many confirmed cases. Additionally, a group of individuals, especially the elderly, believe that everyone’s life is determined and that there is no way to change it. People who live in deprived and rural areas around cities cannot think about changing their lifestyle or their surroundings. Therefore, they not only do not fight COVID-19 but also are indifferent to the mortality rate of this disease so that they can free themselves from their miserable lives, per se. In other words, subjective evaluation of the self from the quality and results of their behaviors depends on evaluations, expectations, and mental norms. Also, people’s behaviors depend on two factors of motivation and the ability to control the behaviors based on subjective assessment of the people (controlling the perceived behavior). In case of enough real control over behaviors and sufficient opportunities, the individual has enough willpower to perform a behavior. Similarly, Rajpura and Nayak (2014) have shown that preceding the illness, positive thoughts regarding the treatment of blood pressure are accompanied by the following treatment [29].
Perception, on the one hand, creates beliefs, and on the other hand, it is made via clear and correct information. However, information alone is not enough. It can help increase healthcare behaviors when it is turned into a belief and then an attitude. Accordingly, information, beliefs, and attitudes are the main essence of motivating people to perform healthy behaviors [30, 31]. The third and fourth factors in following the protocols were social and cultural. These findings agree with Rajjpura and Nayak, Mousavi et al., Siabani, and Mohammadi et al. [29, 30, 32, 33].
Perception of the illness in cultural and socio-economic situations can impact the following differently. For instance, Mousavi et al. have shown in their study that following treatment depends on familial and social support becomes a challenge for the person and results in their ignorance toward healthy behaviors [30]. It seems that culture sets the norms and limits of content approaches and managerial processes, thereby affecting the following protocols via acceptance or unacceptance of factors. The fifth result was regarding media. This result is in line with Wright and Fancourt and Ahmidian and Haghighatian. According to their study, cultural factors and providing information can predict responsive policies [13, 17]. In analyzing these findings, we can argue that all sorts of news are presented via media; media literacy makes viewers choose what to watch and pay attention to which news. One of the reasons for incorrect perceptions is the sending of improper messages, advertisements, and information by several media platforms. Ineffective advertisement and information provision result in the ignorance of a group of people toward COVID-19, thereby not welcoming advertising and information regarding this disease.
In addition, populistic and not scientific information provision about COVID-19 and also delivery of various opinions and scientific and not-scientific hypotheses with contradictions by media and nonexperts results in the eradication of people’s sensitivity toward COVID-19. Also, the dishonesty of government officials and delivering contradictory news by the media made a group of people cynical about the government and mass media platforms, resulting in society’s disbelief. The results of Wright and Fancourt show that an increase in trust in the government effectively confronts the pandemic [13]. Therefore, honest talks by government officials and their timely reflections and reactions by the media can be effective in people’s following health protocols. In addition, people should obtain information via proper and scientific sources regarding COVID-19. However, one of the reasons for not following health protocols during the COVID-19 pandemic might be paying attention to improper and untrustworthy media sources.
Regarding economic factors, two variables of “not having sufficient equipment for examining, screening and finding possible cases of COVID-19” and “interference of recommended protocols with individual and familial interests”, were the most important reasons for not following the health protocols. These findings are in line with the results of Gholamaline et al., Ghiasvanad, and Alizadeh. They have demonstrated that in following drug treatments, various factors such as demographic, social, and economic variables, and factors regarding the healthcare system along with factors regarding the patient are effective [18]. Ghiasvand and Taghizadeh have found occupation and people’s income status effective in following preventive behaviors, along with perceived behavior controls [15]. In analyzing these results, it can be maintained that fighting the COVID-19 pandemic is a sociocultural and economic fight while it is related to the healthcare system. Therefore, controlling this matter requires considering all impacting aspects and all social groups to plan, implement, and evaluate programs for people to follow health protocols and break the chain of prevalence.
Also, in the present study, men used media platforms more than women and married people compared to single ones considered individual, cultural, and media factors effective in following protocols. In addition, people with a university education considered individual, economic, and cultural factors effective in following the protocols. Urban citizens considered cultural and managerial factors effective in following protocols more than rural citizens. Employees found individual, economic, and social factors effective in following the protocols more than people with other types of occupations. These findings are in line with the results of Kharamin et al. Their study shows that women more than men, urban citizens more than rural citizens, married compared to single individuals, educated more than illiterate or less educated individuals, personal characteristics, and so on were effective in following health protocols [34-36]. The benefits of the present study were that almost all influential aspects of ignoring the protocols were gathered in one place and analyzed collectively, and with the use of modern statistical methods, an approach similar yet better than systematic review and thoroughly scientific was made. In addition, the order and importance of each factor that affects following the protocols were obtained.
5. Conclusion
The results of the present study showed that managerial, individual, social, media, economic, and cultural factors affect following the health protocols, and if these factors are not considered by the managers, controlling the pandemic would become harder and impose heavy human, economic, and social costs on the country. Considering the importance of controlling COVID-19 in improving the country’s health and preventing the prevalence of this disease and its implications, managers must consider affective factors in not following the protocols for designing effective programs and interventions. Therefore, by considering the identified factors and designing models based on the factors mentioned above, managers, doctors, and experts should help enhance the following protocols to reduce the negative individual, social, and economic implications.
Study limitations
Some limitations of this study were not participation and limited reception of members of the WhatsApp social media platform members, limited participation of rural citizens, the self-reporting nature of the questionnaire, and the cross-sectional nature of the study. When interpreting the findings of this study, these limitations should be considered. Finally, since the questionnaires were filled out online, it could be possible that the answers are limited to social media platforms. Therefore, the results cannot be generalized to the whole country.
Ethical Considerations
Compliance with ethical guidelines
This study received the following Code of ethics IRARUMS.REC.1399.194. The authors of this study express their gratitude toward members of the faculty and all participants who helped complete and approve the questionnaires and this study.
Funding
School of Health, Ardabil University of Medical Sciences funded this study.
Authors' contributions
The authors equally contributed to this work.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors would like to thank all the professors and university officials of Ardabil University of Medical Sciences, the staff and student of Ardabil University of Medical Sciences, and all the person who participated in the study and helped us in carrying out this research.
References
- Dargahi A, Jeddi F, Vosoughi M, Karami C, Hadisi A, Ahamad Mokhtari S, et al. Investigation of SARS CoV-2 virus in environmental surface. Environmental Research. 2021; 195:110765. [DOI: 10.1016/j.envres.2021.110765]
- Ravaud P, Ouay Fl, Depaulis E, Huckert A, Vegreville B, Tran VT. Reconfiguring health services to reduce the workload of caregivers during the covid-19 outbreak using an open-source scalable platform for remote digital monitoring and coordination of care in hospital command centres. 2020. [Unpublished article] [DOI:10.48550/arXiv.2003.05873]
- Zandian H, Sarailoo M, Dargahi S, Gholizadeh H, Dargahi A, Vosoughi M. Evaluation of knowledge and health behavior of University of medical sciences students about the prevention of covid-19. Work. 2021; 68(3):543-9. [DOI: 10.3233/WOR-203395].
- Pourfarzi F, Rahim Pouran S, Dargahi A, Karami C, Fouladi N, Zandian H, et al. The healthy behaviours and covid-19 mortality among Iranian women: A case–control study. BMC Women's Health. 2021; 21(1):366. [DOI:10.1186/s12905-021-01512-0]
- Vosoughi M, Karami C, Dargahi A, Jeddi F, Jalali KM, Hadisi A, et al. Investigation of SARS-CoV-2 in hospital indoor air of covid-19 patients’ ward with impinger method. Environmental Science and Pollution Research. 2021; 28(36):50480-8. [DOI:10.1007/s11356-021-14260-3]
- Feiz Arefi M, Poursadeqiyan M. [Psychosocial Problems During the COVID-19 Epidemic Crisis (Persian)]. Health in Emergencies and Disasters Quarterly 2022; 7(2):57-8. [DOI:10.32598/hdq.7.2.189.20]
- Cambridge University. Cambridge advanced learner’s dictionary & thesaurus: Definition of observance. London: Cambridge University Press; 2013. [Link]
- Sarailoo M, Matin S, Vosoughi M, Dargahi A, Gholizadeh H, Damavandi MR, et al. Investigating the relationship between occupation and SARS-CoV2. Work. 2021;68(1):27-32. [DOI:10.3233/WOR-205066] [PMID]
- Asayeshi F, Mostafavi F, Hassanzadeh A. [The relation between medication-related beliefs and treatment adherence in patients with hypertension in urban health care centers in Isfahan, Iran (Persian). Journal of Health System Research. 2017; 13(1):32-7. [DOI:10.22122/jhsr.v13i1.2555]
- Kabamba Nzaji M, Ngoie Mwamba G, Mbidi Miema J, Kilolo Ngoy Umba E, Kangulu IB, Banza Ndala DB, et al. Predictors of non-adherence to public health instructions during the covid-19 pandemic in the Democratic Republic of the Congo. J Multidiscip Healthc. 2020; 13:1215-21. [DOI:10.2147/JMDH.S274944] [PMID] [PMCID]
- Graham A, Cullen F, Pickett J, Jonson C, Haner M, Sloan M. Faith in trump, moral foundations, and social distancing defiance during the coronavirus pandemic. 2020. [Unpublished article] [DOI:10.2139/ssrn.3586626]
- Shiloh S, Peleg S, Nudelman G. Adherence to covid-19 protective behaviors: A matter of cognition or emotion? Health Psychology. 2021; 40(7):419-27. [DOI:10.1037/hea0001081] [PMID]
- Wright L, Fancourt D. Do predictors of adherence to pandemic guidelines change over time? A panel study of 22,000 UK adults during the covid-19 pandemic. Preventive Medicine. 2021; 153:106713. [DOI:10.1016/j.ypmed.2021.106713] [PMID] [PMCID]
- Arefi MF, Babaei AP, Barzanouni S, Ebrahimi S, Salehi AR, Khajehnasiri F, et al. Risk perception in the covid-19 pandemic: A health promotion approach. Journal of Education and Health Promotion. 2022; 11:118. [DOI:10.4103/jehp.jehp_1162_21]
- Ghiasvand A, Mohammadtaghizadeh M. [Preventive behaviors toward covid-19 among Iranian people and the factors affecting it (Persian). Iranian Journal of Social Problems. 2021; 12(1):205-37. [DOI:10.22059/ijsp.2021.84971]
- Shahid Chamran University of Ahvaz. [A note by Dr. Marashi; The phenomenon of “adherence” to health advice in the corona epidemic (Persian)] [Internet]. 2020 [Updated 2023 February 2]. Avalable from: [Link]
- Ahmadian D, Haghighatian M. [Sociological analysis of the role of cultural factors on urban environmental behaviors study (citizens of Kermanshah) (Persian)]. Urban Sociological Studies. 2016; 6(18):51-76. [Link]
- Gholamaliei B, Karimi-Shahanjarini A, Roshanaei G, Rezapour-Shahkolaei F. [Medication adherence and its related factors in patients with type ii diabetes (Persian)]. Journal of Education and Community Health. 2016; 2(4):3-12. [DOI:10.21859/jech-02042]
- Dehvan F, Baghi V, Lotfi A, Ghanei Gheshlagh R. [Medication adherence inhibitors and facilitators in type 2 diabetic patients: An integrative review (Persian)]. Scientific Journal of Nursing, Midwifery and Paramedical Faculty. 2017; 3(1):1-17. [DOI:10.29252/sjnmp.3.1.1]
- Naghavi S, Mehrolhassani MH, Nakhaee N, Yazdi-Feyzabadi V. Effective factors in non-compliance with therapeutic orders of specialists in outpatient clinics in Iran: A qualitative study. BMC Health Services Research. 2019; 19(1):413. [DOI:10.1186/s12913-019-4229-4] [PMID] [PMCID]
- Kabusi M, Sepehr P, Pooursadeghian M, Zamani Z, Tahghighi H, Salehi Sahlabadi A, et al. Psychological effects of the outbreak of covid-19 on the mental health of healthcare workers in Iran. Iranian Rehabilitation Journal. 2022; 20(3):379-86. [DOI:10.32598/irj.20.3.1631.1]
- Krejcie RV, Morgan DW. Determining sample size for research activities. Educational and Psychological Measurement. 1970; 30(3):607-10. [DOI:10.1177/001316447003000308]
- Saaty T. Decision making-the analytic of hierarchy and network processes (AHP/ANP). Journal of Systems Science and Systems Engineering. 2004; 13(1):1-35. [DOI:10.1007/s11518-006-0151-5]
- Assefa Y, Gilks CF, Reid S, van de Pas R, Gete DG, Van Damme W. Analysis of the COVID-19 pandemic: lessons towards a more effective response to public health emergencies. Global Health. 2022; 18(1):10. [DOI:10.1186/s12992-022-00805-9]
- Kermani H, Khorshidi M, Araghi Ashtiani M. [The president’s speech: An analysis of covid-19 discourse in the Iranian president’s speeches (Persian)]. Media Studies. 2021; 15(4):112-29. [Link]
- Bailey B, Whelen ML, Strunk DR. Adhering to covid-19 health guidelines: Examining demographic and psychological predictors of adherence. Applied Psychology Health and well-being. 2021; 13(4):968-85. [DOI:10.1111/aphw.12284] [PMID] [PMCID]
- Lee GK, Wang HH, Liu KQ, Cheung Y, Morisky DE, Wong MC. Determinants of medication adherence to antihypertensive medications among a Chinese population using Morisky medication adherence scale. Plos One. 2013; 8(4):e62775. [DOI:10.1371/journal.pone.0062775] [PMID] [PMCID]
- Obreli-Neto PR, Guidoni CM, de Oliveira Baldoni A, Pilger D, Cruciol-Souza JM, Gaeti-Franco WP, et al. Effect of a 36-month pharmaceutical care program on pharmacotherapy adherence in elderly diabetic and hypertensive patients. International Journal of Clinical Pharmacy. 2011; 33(4):642-9. [DOI:10.1007/s11096-011-9518-x] [PMID]
- Rajpura J, Nayak R. Medication adherence in a sample of elderly suffering from hypertension: Evaluating the influence of illness perceptions, treatment beliefs, and illness burden. Journal of Managed Care Pharmacy. 2014; 20(1):58-65. [DOI:10.18553/jmcp.2014.20.1.58] [PMID]
- Mousavizadeh SN, Ashktorab T, Ahmadi F, Zandi M. [Barriers to follow-up in patients with diabetes (Persian)]. Journal of Diabetes Nursing. 2016; 4(3):94-108. [Link]
- Poursadeqiyan M, Kasiri N, Khedri B, Ghalichi Zaveh Z, Babaei Pouya A, Barzanouni S, et al. The fear of covid-19 infection one year after business reopening in Iranian society. Journal of Health Sciences & Surveillance System. 2022; 10(3):284-92. [DOI:10.30476/jhsss.2021.92000.1279]
- Siabani S, Driscoll T, Davidson PM, Najafi F, Jenkins MC, et al. self-care and its predictors in patients with chronic heart failure in Western Iran. The Journal of Cardiovascular Nursing. 2016; 31(1):22-30. [DOI:10.1097/JCN.0000000000000211] [PMID]
- Mohammadi S, Rostamnia D, Kamran A, Savadpour MT. [The relationship between treatment adherence and patients’ drug beliefs and demographic factors (Persian)]. Paper presented at: 6th Annual Student Congress of Student Research Committee of Ardabil University of Medical Sciences. 9 December 1993; Ardabil, Iran. [Link]
- Akintola O, Chikoko G. Factors influencing motivation and job satisfaction among supervisors of community health workers in marginalized communities in South Africa. Human Resources for Health. 2016; 14(1):54. [DOI:10.1186/s12960-016-0151-6] [PMID] [PMCID]
- Hamidzadeh Y, Hashemiparast M, Hassankhani H, Allahverdipour H. [Local-level challenges to implementing health education programs in rural settings: A qualitative study (Persian)]. Family Medicine & Primary Care Review. 2019; 21(1):30-4. [DOI:10.5114/fmpcr.2019.82976]
- Kharamin S, Shakibkhah S, Rafiei M, Mohammad Hosseinpour H. [Evaluation of adherence to quarantine, health related protocols and some associated factors in covid 19 pandemic (Persian)]. Armaghan-e-Danesh. 2021; 25(S1):903-20. [DOI:10.52547/armaghanj.25.S1.903]
Type of Study: Applicable |
Subject:
Special
Received: 2021/02/15 | Accepted: 2022/01/27 | Published: 2022/04/27
Received: 2021/02/15 | Accepted: 2022/01/27 | Published: 2022/04/27
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |





