Volume 9, Issue 1 (Autumn 2023)
Health in Emergencies and Disasters Quarterly 2023, 9(1): 43-54 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Moradi M, Sharififar S, Zareiyan A, Hosseini Shokouh S J, Nasiri A. Advantages of Setting up Temporary Medical Centers in Response to COVID-19 Pandemic: A Qualitative Study. Health in Emergencies and Disasters Quarterly 2023; 9 (1) :43-54
URL: http://hdq.uswr.ac.ir/article-1-516-en.html
URL: http://hdq.uswr.ac.ir/article-1-516-en.html
Maryam Moradi1 

 , Simintaj Sharififar *2
, Simintaj Sharififar *2 

 , Armin Zareiyan1
, Armin Zareiyan1 

 , Seyyed- Javad Hosseini Shokouh3
, Seyyed- Javad Hosseini Shokouh3 

 , Ali Nasiri4
, Ali Nasiri4 




 , Simintaj Sharififar *2
, Simintaj Sharififar *2 

 , Armin Zareiyan1
, Armin Zareiyan1 

 , Seyyed- Javad Hosseini Shokouh3
, Seyyed- Javad Hosseini Shokouh3 

 , Ali Nasiri4
, Ali Nasiri4 


1- Department of Health in Disaster and Emergencies, School of Nursing, Aja University of Medical Sciences, Tehran, Iran., Aja University of Medical Sciences, Tehran,
2- Department of Health in Disaster and Emergencies, School of Nursing, Aja University of Medical Sciences, Tehran, Iran. ,s.sharififar@yahoo.com
3- Department of Infection & Tropical Disease, Infections Disease Research Center, Faculty of Medicine, Aja University of Medical Sciences, Tehran, Iran., Aja University of Medical Sciences, Tehran,
4- Department of Health in Disaster and Emergencies, School of Health, Baqiyatallah University of Medical Sciences, Tehran, Iran., Baqiyatallah University of Medical Sciences, Tehran, Iran
2- Department of Health in Disaster and Emergencies, School of Nursing, Aja University of Medical Sciences, Tehran, Iran. ,
3- Department of Infection & Tropical Disease, Infections Disease Research Center, Faculty of Medicine, Aja University of Medical Sciences, Tehran, Iran., Aja University of Medical Sciences, Tehran,
4- Department of Health in Disaster and Emergencies, School of Health, Baqiyatallah University of Medical Sciences, Tehran, Iran., Baqiyatallah University of Medical Sciences, Tehran, Iran
Full-Text [PDF 537 kb]
(992 Downloads)
| Abstract (HTML) (2902 Views)
Full-Text: (790 Views)
Introduction
The coronavirus disease 2019 (COVID-19) outbreak started at the end of 2019 in Wuhan, China [1, 2]. The virus’s long incubation period and its unusual symptoms, with the dysfunction of various organs, led to a heightened infection rate and mortality. The resultant pandemic strained healthcare systems with hospital bed shortages and high admission of patients to hospitals [3].
An acute scarcity of resources and facilities has also been experienced at the global level in the SARS, MERS, and COVID-19 epidemics and pandemics [4, 5]. Outbreaks of diseases can have destructive consequences, such as high mortality and social/economic dysfunction, paralyzing health system infrastructures. Consequently, quickly responding to these disasters is important in reducing these fallout [6].
Countries like China initially implemented home quarantine measures for patients with mild symptoms. However, the outbreak of COVID-19 among family members became one of the main ways of virus transmission. As a result, this method failed to control the pandemic and mortality [1, 7]. Drawing upon previous experiences about the control of epidemics and mortality and also taking into account the recommendations of the World Health Organization (WHO) [8], most countries, such as Iran, adopted the policy of converting sports and exhibition venues into temporary hospitals and treatment centers to admit patients with mild symptoms.
Shu et al. argued that temporary centers are necessary to treat patients with COVID-19. They are also suitable responses to the shortages of hospital beds. They increase the capacity of patient admission, provide efficient care to patients, and prevent the progression to a critical situation [9].
Numerous temporary hospitals have already been set up worldwide in response to epidemics and pandemics such as influenza [10] and COVID-19 [11, 12]. The experiences of these centers regarding the implementation of rapid measures, diagnosis and disease control, and mortality reduction have also been published, especially in China [13] and America [11].
In Iran, after the first experience with the intensification of the COVID-19 epidemic, such centers under the name of convalescence were requested in several cities in early 2020. They were charged for caring for the patients after partial recovery. These centers were temporarily set up in different parts of the country. Most of their activity was during the peak of the COVID-19 pandemic, and they lacked a permanent activity. Unfortunately, there are no specific reports and statistics on the performance and activity of these centers. Military and government organizations set up these convalescences. The first army convalescent home was established on March 14, 2019, in Pardisan City of Qom Province, Iran, with a capacity of 400 beds. Later on, a 2000-bed military center was launched. Universities of medical sciences and the Revolutionary Guards have set up similar centers with different capacities for accepting patients. For example, Iranmal convalescence, under the supervision of Iran University of Medical Sciences, provided services to 123 patients during 51 working days. Shahid Beheshti University of Medical Sciences identified three places to construct convalescent homes under its control. Due to the importance of time in this case, a closed clinic was used to build the first convalescent center with 70 beds. Also, Sorkheh Hesar and Khaqani convalescent centers were established in the crisis management sheds of the municipality, each with a capacity of 60 beds and equipped with medical supplies to complete the process of serving patients [14].
Considering the advantages of these centers, they can be used in the design and operation of temporary medical centers. According to our knowledge, there is limited information on the performance and advantages of temporary medical centers during the COVID-19 pandemic. As a result, this qualitative study aims to determine the temporary medical centers’ advantages in response to the COVID-19 pandemic.
Materials and Methods
This qualitative research in Iran employed a content analysis approach. Between March and July 2021, in-depth and semi-structured interviews were conducted with people actively involved in managing the COVID-19 pandemic. The participants included patients, experts in construction, and equipment and maintenance specialists. The participants were working in the temporary medical centers. They had a history of dealing with biological agents in the Tehran emergency health system. This group comprised combat medicine managers, non-operating defense experts, disaster reduction offices, and operation and crisis experts with at least one year of work experience in this field. The inclusion criteria were a willingness to participate in the study, effective communication with the interviewer, and informed consent. The exclusion criterion was an inability to continue with the research.
This study employed a combination of purposeful, snowball, and theoretical samplings [15]. Purposeful sampling guided the selection of the interviewees. The theoretical sampling determined the number of people, required data sources, and the study objectives. This type of sampling with rich information helps investigate and analyze the nature and dimensions of the phenomenon better [16]. The snowball sampling was used to identify experts other than those initially participating in the study. Therefore, by preparing a sampling matrix, 22 experts were selected with maximum variation, considering criteria such as work experience, age, gender, and education level. Three patients hospitalized in temporary medical centers were also included in the study.
During the interview, the researcher first introduced herself, briefly explained the objectives and significance of the study, and assured the participants about the confidentiality of their personal information. Ethical considerations were observed throughout the study, and informed consent was obtained from the participants for entering the analysis and recording of interviews. Face-to-face and semi-structured interviews were conducted with the participants in a secure environment, lasting 60 to 90 minutes and continuing until data saturation was achieved. The interviews concluded when the interviewees felt tired; answering the questions was not compulsory.
The interview questions were expanded, revised, and formulated after reviewing the literature, conducting 3 preliminary interviews (pre-test to confirm the reliability of the questions), and holding three meetings with the research team. The primary questions were asked at the beginning of the interview, and the additional questions were posed according to the participants’ responses. The interviews were transcribed verbatim at the earliest opportunity, and the conventional content analysis method proposed by Graneheim and Lundman was used to analyze the data. Coding and analyzing the data were done simultaneously after reading the interviews several times and immersing in the contents facilitated by MAXQDA software. In this way, the words and key phrases were specified and labeled as descriptive codes (examples). Subsequently, the initial codes were revised and labeled as analytical codes through higher-level abstraction. After modification, they were defined as interpretive codes (themes) [17, 18]. Then, the codes were categorized into different classes based on their similarities and differences [19].
Data trustworthiness
The quality of results was confirmed against the Guba and Lincoln criteria [20]. To increase the study’s credibility, the researchers observed the principle of diversity in sampling. At the end of each interview, the interviewer’s general understanding of the subject’s statements was briefly expressed and approved by the subject. Also, after completing the coding process and data analysis, a table of themes, subthemes, and codes, along with the participants’ quotes, was presented to 6 participants for confirmation and approval. To obtain confirmability, the researchers sent the result of data analysis along with the findings to 4 top researchers in the field of qualitative research and 5 experts and managers of temporary health centers. The necessary corrections were made according to their comments while maintaining the authenticity of the results and data. Raw data and all notes were kept for revisions at a later time. All available team members were involved in the analysis and coding process to increase the dependability. They were encouraged to express their opinions in the meetings held with them. In the end, the names of the themes and subthemes were finalized with the approval of the research team. To increase the transferability, a complete description of the entire research process was provided, the participants’ quotes were presented, and the study findings were sent to 5 people who met the inclusion criteria but did not participate for confirmation.
3. Results
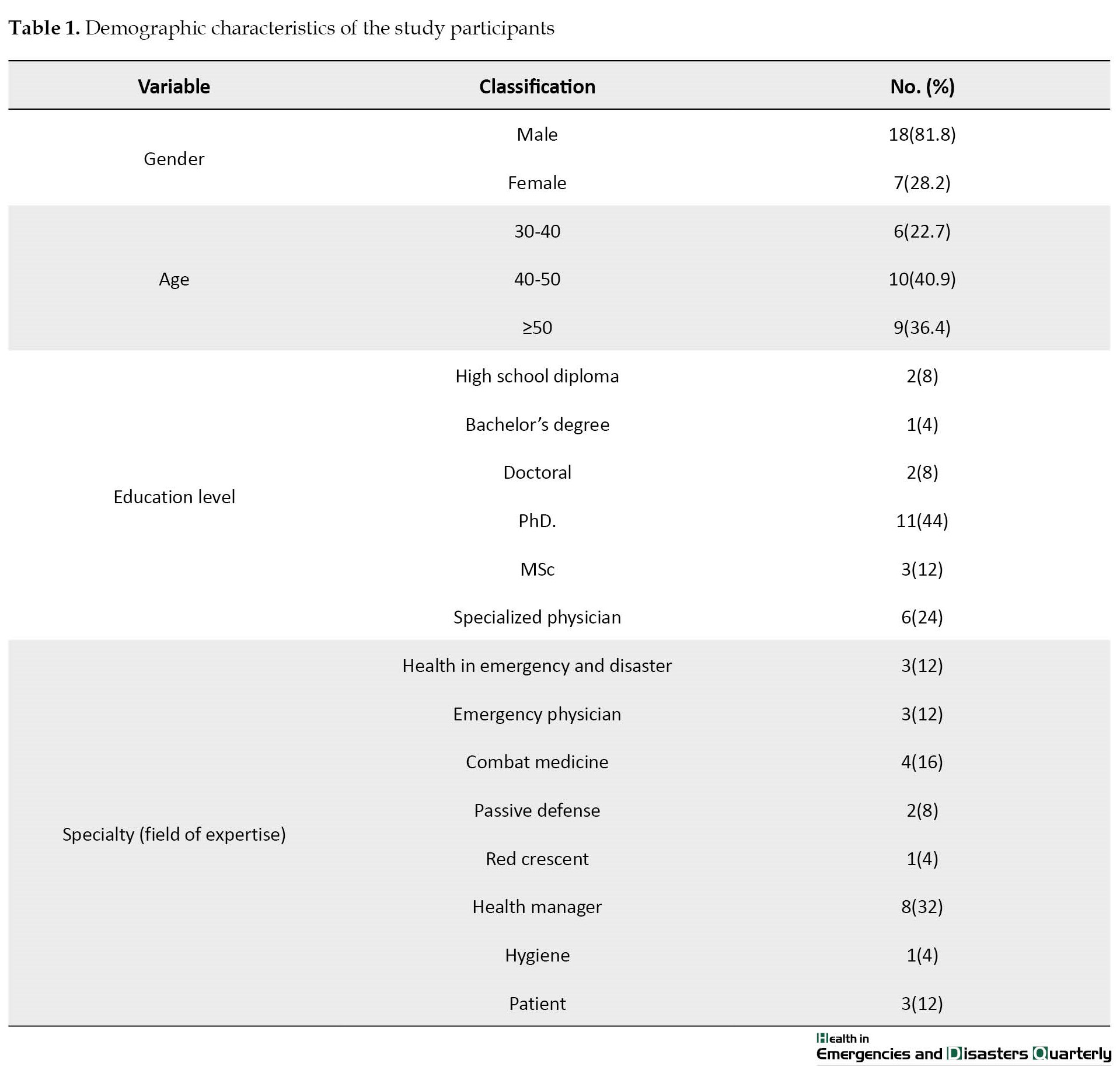
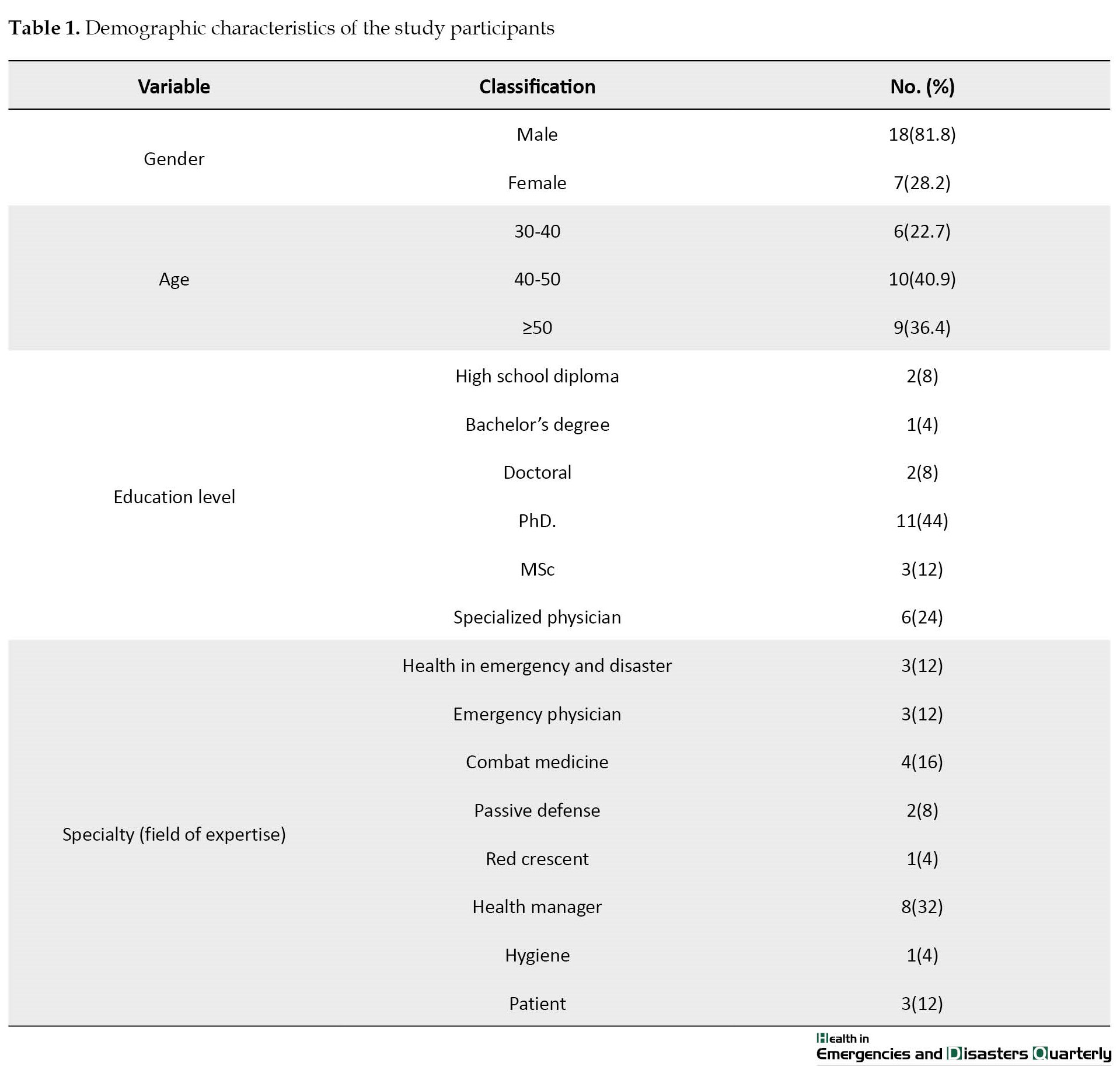
Most study participants were male, had a PhD, and were specialized in health management. Three patients hospitalized in temporary health centers had high school diploma or Bachelor’s degree (Table 1).
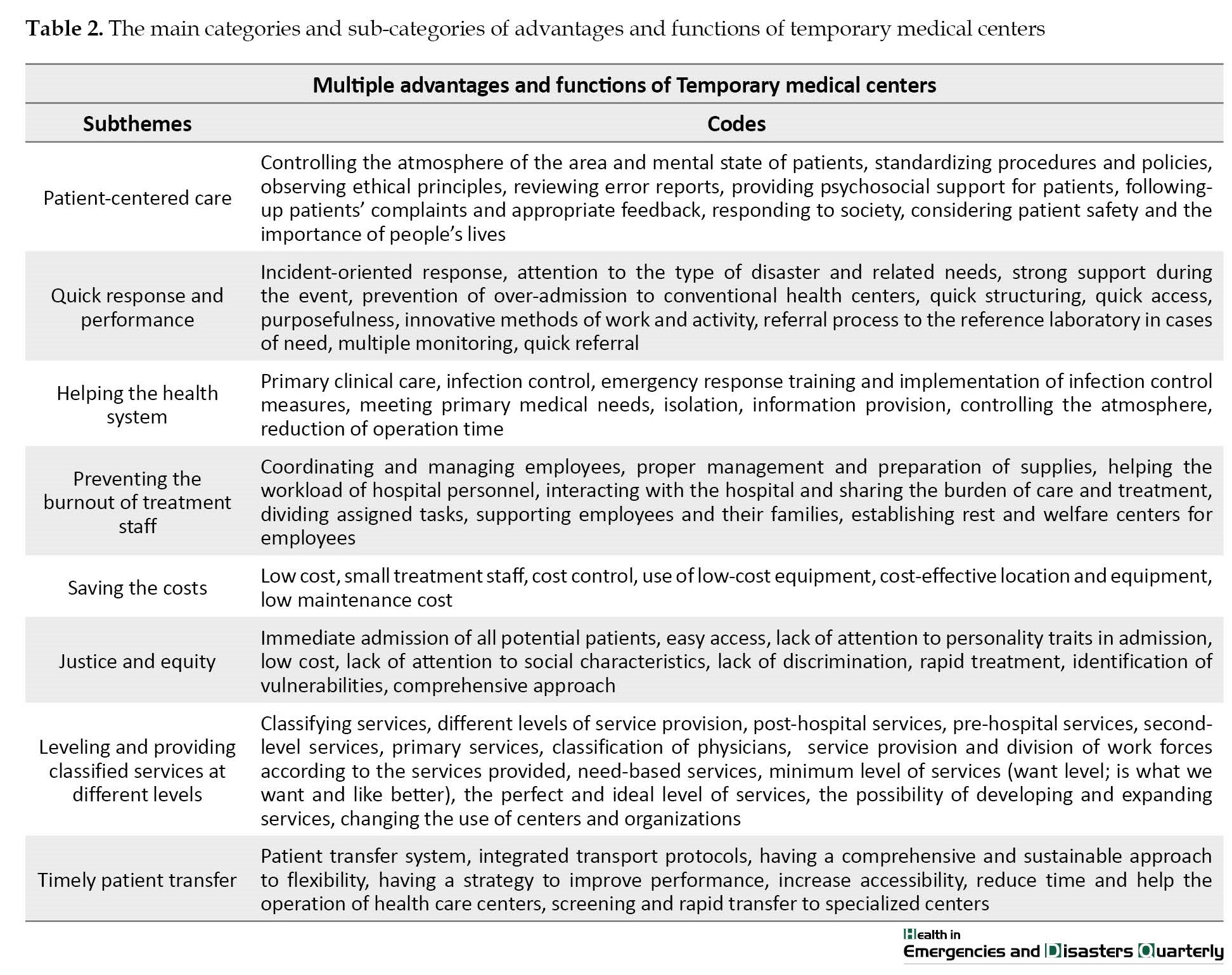
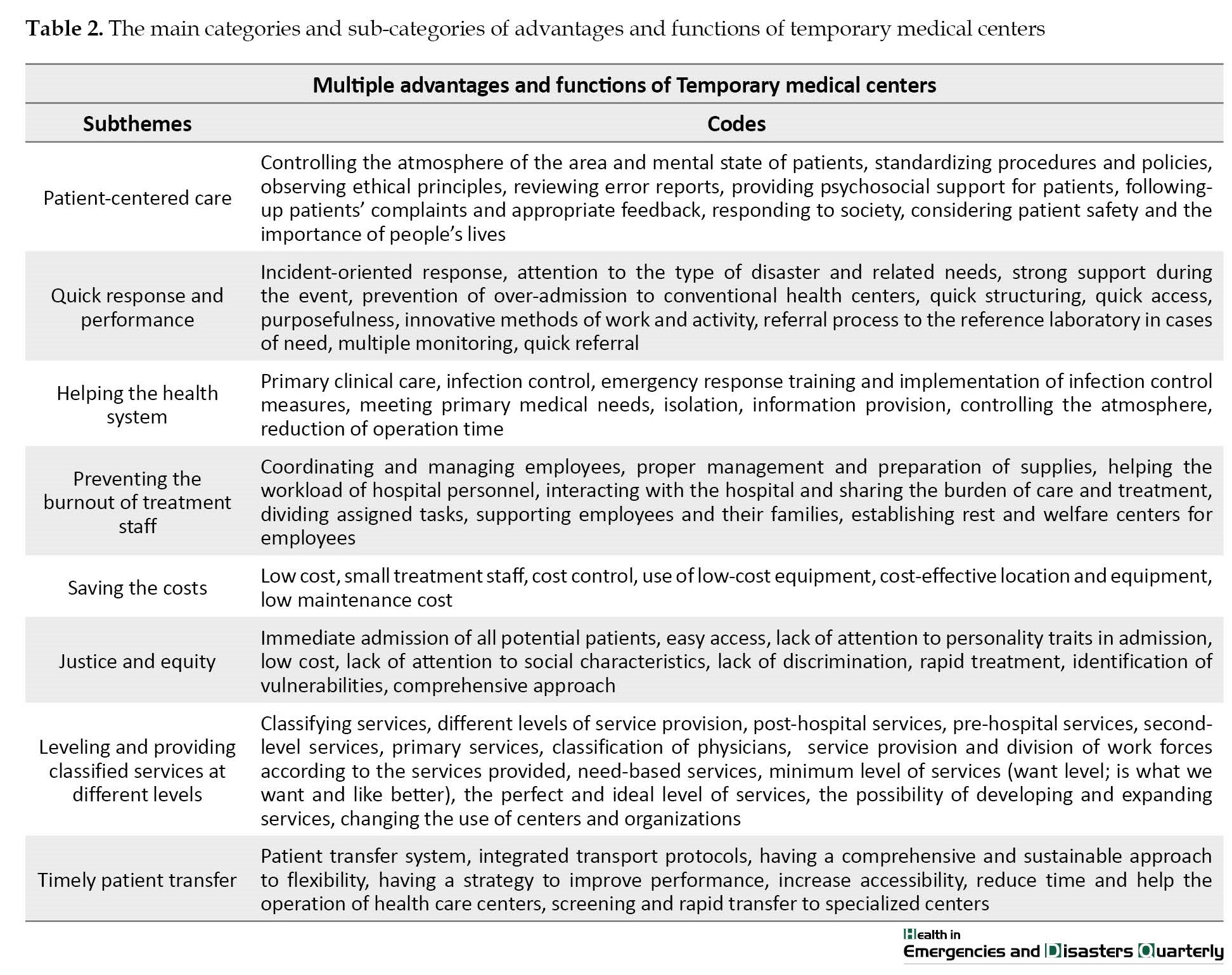
According to the results, despite the problems and limitations, temporary medical centers have many advantages and positive functions, which emphasize the importance of these centers in policies and programs. Multiple advantages and functions of temporary medical centers can be classified into 8 subthemes (Table 2).
Multiple advantages and functions
Resource management, including human resources, is one of the most important components of preparation and performance in response to the COVID-19 pandemic. Establishing temporary medical centers significantly reduces disasters’ negative impact and saves human lives. These centers can act as protectors in times of crisis, and due to limitations in human resources and the urgency of intervention, they can provide much-needed care and medical interventions to the public. Although these centers encounter many challenges and constraints, they possess several advantages and positive functions, which have been classified into 8 subthemes in this study: patient-centered care, quick performance and response, helping the health system, preventing the burnout of treatment staff, savings the costs, justice and equality, leveling and providing classified services at different levels, and timely patient transfer.
Patient-centered care
One of the most important issues in temporary medical centers is the patient-centered care. Because these centers are built with specific goals, they show the highest level of effectiveness in times of crisis with the least paperwork and administrative bureaucracy. In normal conditions, according to the management of resources, regulations, and standards, a lot of time is spent on paperwork and other bureaucratic procedures in hospitals. However, this time is minimized in temporary medical centers, and the focus is on providing essential care. The main goal of these centers is to mitigate problems, treat patients, and control the atmosphere by using all-around support. Although there are no standard and listed structures in many cases, patients’ complaints and feedback are considered. Compliance with ethical principles is a basic criterion in establishing and operating these centers. In interviews with experts, control of the atmosphere in the region, treatment of patients, standardization of procedures and policies, compliance with ethical principles, review of error reports, psychosocial support of patients, follow-up of patient’s complaints, and appropriate feedback, accountability to society, patient safety and the importance of people’s lives were the most important factors mentioned.
“When we took action to control the Coronavirus, the situation completely changed, and we felt that a kind of peace returned to the society because people saw that healthcare workers are trying to provide the necessary care to people as quickly as possible” (Interviewee No. 3).
“You see, all measures taken in these centers are for public health and based on ethical philosophy. They were trying to get people treated quickly by providing patient-centered care and treatment while observing ethical principles. They were trying to provide patients the highest level of treatment” (Interviewee No. 9).
Quick performance and response
One of the most important features of temporary medical centers is the quick performance and response of these centers to crises. Considering that these centers are set up in response to crises, immediate reaction should be one of the essential characteristics of these centers. These centers should have the highest and best possible answer to the crisis immediately. A quick and correct response requires strong planning and management, though sometimes this quick response may lead to mistakes. However, according to their mission, these centers try to minimize errors. Usually, these centers are opened when society needs quick action and response. They also help other institutions and departments involved in the incident. The incident-oriented response, attention to the type of disaster and related needs, provision of strong support during the event, prevention of overload to conventional hospitals, quick structuring, prompt access, purposefulness, innovative methods of work and activity, referral to the reference laboratory in cases of need, multiple monitoring, and immediate referral were the most important factors mentioned by the interviewees.
“For example, temporary medical centers can be partly or completely relocated. They can also be set up in a building with a very different use. The mobility and speed of actions when setting up medical centers and even moving and deploying employees in the required places are also high in these centers” (Interviewee No. 17).
Helping the health system
Events and crises create many challenges for the health system in any country. Depending on the type of event, the health system bears the greatest responsibility. Typically, the health systems could not deal with these crises in most cases because of their facilities and human resources limitations. On the other hand, the suddenness of the crisis and its unknown consequences require an immediate and accurate response, which is practically impossible in the first hours of the crisis. If the health system is not supported, it may disintegrate under enormous pressure. Temporary medical centers provide the highest level of help to the health system because they take over part of the duties of hospitals and transfer only urgent and emergency cases to hospitals using a screening system. Among the most important codes extracted in this study, we can refer to the provision of basic clinical care, infection control, training of emergency measures, implementation of infection control measures, meeting basic medical needs, isolation, information provision, control of the atmosphere, and reduction of service delivery time.
“Sometimes, the establishment and operation of a center take away a large amount of pressure from hospitals and help them to treat acute cases more carefully. These centers are helpful as they provide primary clinical care and correct information” (Interviewee No. 6).
Preventing the burnout of treatment staff
Job burnout has been one of the main problems of medical staff in recent years. Many studies have explored the burnout of medical staff and showed a high burnout among healthcare workers. Job burnout may surge in a crisis like a biological event due to its social and psychological consequences, which leads to other problems. One of the solutions to the problem of burnout in medical staff and to reduce the work pressure is the establishment of temporary hospitals and medical centers and the use of trained volunteers. Coordination and management of employees, appropriate management of the supplies, reduction of workload in hospital personnel, interaction with the hospital, sharing of care and treatment duties, support of employees and their families, and establishment of the rest and welfare centers for treatment staff were the most important codes extracted from the participants’ statements. According to the instructions of these centers, the interaction between treatment staff and even between personnel and management teams should be continued, and the employees should be comfortable in expressing their opinions and wishes. This simple act helps treatment staff to keep their morale and vitality. This measure can also minimize the job burnout of treatment staff.
“We saw how happy the hospital staff were about establishing these centers, and sometimes they personally came and thanked us and said that if it wasn’t for you, we couldn’t have been able to handle the public demand, and maybe we would have given up” (Interviewee No. 4).
Saving the costs
Heavy medical expenses are one of the main problems that should be considered in times of crisis. Due to the unknown nature of diseases and events, many diagnostic and treatment measures should be taken at the outset. Suppose appropriate and practical steps are not thought out for times of crisis, and we do not have relevant policies for these times. In that case, we will incur high social and economic costs, and the expected results will be minimized. Setting up temporary medical centers during the COVID-19 pandemic is an appropriate policy, which greatly reduces unnecessary costs and helps the health system cope with public demand in times of crisis. In addition to the macro level, at the community level, these centers help individuals and families receive the same treatments and care they would receive in normal hospitals at a much lower cost and in a shorter time.
“Well, one of the duties of public centers is to respond to crises or disasters. However, it is not always possible to respond to these crises easily because the income does not match the expenses, and it is not cost-effective for private centers to have dual-purpose equipment. These centers have a plan but are less extensive than public hospitals. Hospitals also have high expenses during a crisis, so these centers help save the costs” (Interviewee No. 10).
“If you compare the cost of treatment in these centers and normal hospitals, you will see a big difference, so they are very helpful. People immediately go to these centers after getting infected because they have easy access. People either get treatment or at least information on where to go” (Interviewee No. 1).
Justice and equality
Justice and equality are two key and frequent concepts seen in the literature of all fields in recent years. Despite the importance of these two concepts, the difference between them is still debatable. Justice in health means treating all people based on their needs and conditions in such a way that makes even the situation. However, equality refers to equal treatment for everyone regardless of the situation. In times of crisis and events, both concepts are important. Under normal conditions, people with better financial status use more and better facilities and can get admitted to hospitals with more equipment. Still, people with lower social and economic status may be unable to use the necessary facilities and often do not get what they need. However, this disparity is not acceptable in a crisis. These centers provide equal services to everyone in need, regardless of their social and economic status. This action is equivalent to justice in health care access for all society members. In the biomedical field, having access to and benefitting from quality services, and in the social field, offering financial support for service users, especially the needy and people with low incomes, are the goals of justice in the healthcare system. Access to services should be easy, team-based, continuous, integrated with appropriate technology, and available for all age and gender groups. Health systems should ensure that all people can access health services in their nearest residence, benefit from these services at times of need, and are financially protected.
However, at the time of biological events, hospitals may intentionally ignore justice and equality in access and service delivery and provide unequal services to people in a targeted manner, considering their facilities and the situation. Therefore, justice and equality can be specific to these centers; in other words, temporary medical centers provide services to all patients needing treatment regardless of their differences. Among the codes extracted in this study were immediate admission of all potential patients, easy access, no attention to personality traits in admission, low cost, lack of attention to social characteristics, no discrimination, quick treatment, detection of vulnerabilities, and holistic approach.
“... Now, a person with money can easily go to a private hospital with the best facilities and get faster and better treatment, but what about the poor people in the city or countryside? They sometimes do not have access to even minimum care, which is injustice. This condition means inequality in access, inability to purchase services, and unavailability of health services. However, temporary medical centers can provide basic facilities even in low-income places, and we can say that they look at everyone equally. For them, everyone’s health is important, not the health of a few...” (Interviewee No. 13).
Leveling and proving classified services at different levels
One of the temporary medical centers’ main advantages and functions is the possibility of leveling services. Hospitals and conventional health centers are set up with a fixed purpose; changing this purpose is impossible or requires a lot of money. Temporary medical centers can operate at different levels of service delivery based on different situations and needs in times of crisis. As primary screening centers, they can remove the burden of hospitals. They also play a comparable role with hospitals and provide all the necessary services to needy people. After receiving the main services in the hospital, people can receive post-hospital services in these centers. These services facilitate the continuation of the treatment process as well as rehabilitation. It should be noted that in crises and biological incidents, these centers mostly play a prehospital role. By screening and providing primary services and referrals, they play a significant role in helping hospitals and the healthcare system. Furthermore, health promotion, prevention, treatment, and rehabilitation services are integrated into these centers as comprehensive services delivered to people who need them. Different levels of service provision, post-hospital services, second-level services, primary services, grouping of physicians, service provision and division of workforces according to services, need-based services, minimum service level, want level (what we want and like to be better), perfect and ideal levels, the possibility of developing and expanding services, and changing the use of centers and organizations were among the extracted codes related to this subtheme.
“Most of the post-hospital services are provided here. Prehospital services can also be considered as triage. If patients are considered outpatients, they will receive medication; if they are seriously ill, they will be sent to the designated hospitals. Specialists are constantly present in prehospital centers, but specialists can be on-call in post-hospital centers. This system is like a chain of service provision. The patient’s file is created in the outpatient clinic, and if he needs inpatient care, he will be referred to the hospital” (Interviewee No. 14).
“If we want to level the services based on needs, one of these levels is the minimum level (must level), which means that we cannot ignore it. One level higher is the want level, which indicates what we want and like to be better. Another level is the perfect and ideal level, which depends on the conditions and facilities and at which level you want to develop this platform”(Interviewee No. 17).
Timely patient transfers
The last subtheme related to the advantages and functions of temporary medical centers is swift patient transfer. This subtheme is considered one of the basic components of service provision in the health system, which can vary in different conditions. Access to medical centers and service delivery is one of the most influential topics in this field. An immediate transfer and providing appropriate and timely service refer to simple access to the desired center and patients’ transfer to them as soon as possible. Since the temporary medical centers are established in a targeted manner and specific places, two points should be considered in setting up these centers. First, they should be set up in areas with the least access to health and medical centers. Second, they should be set up in places with easy and quick access to other centers and hospitals. In other words, these centers act as a bridge between people needing treatment and hospitals. Patient transfer system; integrated transport protocols; a comprehensive and sustainable approach for flexibility, screening, and rapid transfer of patients to specialized centers; and having a strategy to improve performance, increase accessibility, reduce time, and help the operation of health care centers were the most important codes extracted about this sub-theme.
“... Access to care should be provided for people in all places, and there should be no need to transfer patients from one place to another because this drawback is the basis for the transmission of virus from one place to another” (Interviewee No. 12).
“The capacity created in the outpatient department to work effectively is important regarding access and not requiring patient transfer to other places. So, these centers should be set up in different parts of the city and be able to manage patients without transferring unnecessary cases to higher levels of services” (Interviewee No. 16).
Discussion
Throughout human history, infectious diseases such as plague, SARS, COVID-19, and influenza have greatly threatened human health, leaving millions dead. However, humans have dealt with these diseases by isolating infected people and breaking the cycle of infection [21-23]. Due to the inadequate resources in some countries, they have decided to build temporary health centers by converting different venues and hotels into temporary medical centers. This study aimed to highlight the advantages and performance of temporary medical centers in response to the COVID-19 pandemic.
We found that temporary medical centers have many advantages, such as immediate admission of all potential patients and easy access to health services regardless of personality traits. These centers have certain characteristics, such as low treatment costs, not considering social characteristics, lack of discrimination, and fast treatment. In general, establishing temporary medical centers effectively controls infectious diseases when the resources are scarce. By admitting patients with mild symptoms, temporary medical centers reduce the transmission of the virus and, as a result, the number of new cases. The experiences of China in fighting the COVID-19 pandemic indicate that temporary centers should provide people with easy access to health care [3, 24]. Although previous studies have shown that temporary centers should be close to key organizations, this proximity may increase disease transmission [25].
Temporary medical centers with specific standards, procedures, and policies control infection and treat patients in areas with high disease prevalence. By complying with moral principles and providing psychological and therapeutic support, these centers can respond to the needs of society in times of crisis. In line with the present study’s findings, previous studies have also shown that temporary hospitals should accept patients with mild symptoms, ensure their safety, and pay attention to their social and emotional needs [3]. The use of volunteers or untrained staff affects the quality of services. Experiences of temporary centers in China indicate that the employees and workforce should be selected in a way that guarantees the safety, quality, and efficiency of care services [26].
Other relevant studies have referred to factors such as monitoring of nurses, standardization of equipment, disinfection of the environment, reducing patients’ fear and anxiety, and strengthening emotional interaction between patients and physicians as the necessity of running temporary medical centers [24, 27]. Some studies have referred to developing protocols, instructions, and processes in response to COVID-19 in these centers [1, 28]. It is necessary to develop clinical protocols to manage patients in critical conditions, evaluate new symptoms, and manage staff. These protocols have been adopted from the standard care of the hospital system, the consensus of experts, and recommendations of disease control and prevention centers [11].
The present study showed that after being quickly established in a targeted manner, temporary treatment centers could increase the chances of patients’ recovery, provide primary clinical care and screening, help identify severe cases in the early stages, and refer them to the hospital. Moreover, by providing strong support, meeting patients’ basic medical needs, isolating infected cases, and conducting necessary tests and monitoring, these canters can reduce the number of hospital admissions and visits to healthcare centers. They can also reduce the workload of hospital staff by providing emergency measures, implementing infection control policies, sharing information, controlling the atmosphere, reducing operation time, and using low-cost equipment with low maintenance costs, which reduces treatment time and costs. Previous studies have shown that the number of physicians can be reduced in temporary treatment centers, as they mostly treat people with mild symptoms. By improving management efficiency, they can reduce costs and the need for human resources [7, 29]. However, due to these centers’ lack of specialized equipment, they should identify critically ill patients and refer them to hospitals as soon as possible [30].
Also, underlying diseases of elderly patients were managed in these centers, and counseling was offered to all patients if they wished. Several activities were also considered to relax the patients and improve the relationship between the patient and the doctor [26].
Previous studies have underscored understanding and respecting the customs of patients and local staff in these centers. This measure would promote communication and coordination between staff with different cultural backgrounds and provide the best patient care [31]. Cultural norms, special customs, non-acceptance of instructions, and mistrust of people in these centers can affect their operation and success [32]. The fear of families and health workers being exposed to the disease is also one obstacle for temporary medical centers.
Previous studies have considered it necessary to fully understand and respect the customs of patients and local staff in these centers, which would promote communication and coordination between staff with different cultural backgrounds and provide the best patient care [33].
Similar to our results, previous studies categorized the outcomes of establishing temporary medical centers. The first outcome is accelerating the diagnosis and increasing the recovered cases that showed initial effects on controlling the COVID-19 pandemic. The second outcome refers to a rapid increase in discharged patients, admissions, and treatment in temporary centers. This outcome also shows the control effects of the centers. In the third outcome, the COVID-19 pandemic showed a significant improvement. The last group of these centers achieved regular success in controlling the pandemic and played an important role in defeating the COVID-19 pandemic [34].
Among the advantages of temporary medical centers identified in the present study, we can refer to information management, integrated patient transport protocols and systems, and strategies to improve performance and increase accessibility. One of the most important aspects of disaster and emergency response is to ensure effective, frequent, and timely information exchange. In setting up temporary treatment centers, it is vital to pay attention to information management and discussion, so the management of these centers should be based on the information and communication management system [35, 36].
Among other benefits of temporary medical centers, we can point to the success in performing assigned tasks, coordination and management of employees, proper management and preparation of supplies, interaction with referral hospitals, the existence of support for employees and their families, the establishment of rest and welfare centers for employees, and prevention of job burnout. Previous studies on the response to biological attacks have pointed out problems related to quarantine, primary medical care, and daily management of patients. They have emphasized the importance of a quick response management system, creating a disease management team, and forming an appropriate medical structure [7]. Previous studies also considered the lack of proper planning as a major challenge of temporary medical centers [6, 36, 37].
Conclusion
The COVID-19 pandemic has led to an unprecedented health and economic crisis with profound and multifaceted consequences worldwide. Securing the operation of health centers to deal with the spread of such a highly contagious and deadly disease has been the top priority of many governments. One of the key elements to reduce the overload of care in large hospitals during peak health emergencies is the development of flexible policies for admitting many patients. These temporary centers, with specific criteria for accepting patients, ensuring their safety in care, helping to break internal transmission, and paying attention to the social and emotional needs of patients, as a rapid response mechanism, can respond to the current COVID-19 pandemic as well as other epidemics in future. The result of this study can be used in managing biological emergencies in the future because it provides a clear picture of the multiple advantages and functions of temporary medical centers.
Limitations
According to the characteristics of qualitative research, the generalization of the results of this study is limited only to the study environment. Therefore, conducting similar studies in other departments is recommended. Gaining access to experts was another limitation in this study, but interviews were conducted with key stakeholders. Another limitation of this study was its coincidence simultaneity with the COVID-19 pandemic. The limited interview time due to the busy work schedule and working in management positions of some participants was also a limitation of this study.
Ethical Considerations
Compliance with ethical guidelines
The present study was approved by the Iran Army University of Medical Sciences (Code: IR.AJAUMS.REC.1400.254). To comply with the ethical principles in the research, written informed consent was obtained from the participants, and the interview time was organized with them. All participants were told about the voluntary nature of participation in the study and to withdraw from the interview at any time. The interview process and how to publish the results were also explained to the participants, and they were assured that their names would remain confidential in publishing the results.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Conceptualization, supervision and data analysis: Maryam Moradi and Simintaj Sharififar; Methodology: Maryam Moradi, Simintaj Sharififar and Armin Zareiyan; Data collection: Maryam Moradi; Funding acquisition, resources, investigation, and writing: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors thank all the participants of the interview process for giving their valuable time and cooperation. In addition, the authors would also like to extend their gratitude to anonymous reviewers for their helpful comments and suggestions.
References
The coronavirus disease 2019 (COVID-19) outbreak started at the end of 2019 in Wuhan, China [1, 2]. The virus’s long incubation period and its unusual symptoms, with the dysfunction of various organs, led to a heightened infection rate and mortality. The resultant pandemic strained healthcare systems with hospital bed shortages and high admission of patients to hospitals [3].
An acute scarcity of resources and facilities has also been experienced at the global level in the SARS, MERS, and COVID-19 epidemics and pandemics [4, 5]. Outbreaks of diseases can have destructive consequences, such as high mortality and social/economic dysfunction, paralyzing health system infrastructures. Consequently, quickly responding to these disasters is important in reducing these fallout [6].
Countries like China initially implemented home quarantine measures for patients with mild symptoms. However, the outbreak of COVID-19 among family members became one of the main ways of virus transmission. As a result, this method failed to control the pandemic and mortality [1, 7]. Drawing upon previous experiences about the control of epidemics and mortality and also taking into account the recommendations of the World Health Organization (WHO) [8], most countries, such as Iran, adopted the policy of converting sports and exhibition venues into temporary hospitals and treatment centers to admit patients with mild symptoms.
Shu et al. argued that temporary centers are necessary to treat patients with COVID-19. They are also suitable responses to the shortages of hospital beds. They increase the capacity of patient admission, provide efficient care to patients, and prevent the progression to a critical situation [9].
Numerous temporary hospitals have already been set up worldwide in response to epidemics and pandemics such as influenza [10] and COVID-19 [11, 12]. The experiences of these centers regarding the implementation of rapid measures, diagnosis and disease control, and mortality reduction have also been published, especially in China [13] and America [11].
In Iran, after the first experience with the intensification of the COVID-19 epidemic, such centers under the name of convalescence were requested in several cities in early 2020. They were charged for caring for the patients after partial recovery. These centers were temporarily set up in different parts of the country. Most of their activity was during the peak of the COVID-19 pandemic, and they lacked a permanent activity. Unfortunately, there are no specific reports and statistics on the performance and activity of these centers. Military and government organizations set up these convalescences. The first army convalescent home was established on March 14, 2019, in Pardisan City of Qom Province, Iran, with a capacity of 400 beds. Later on, a 2000-bed military center was launched. Universities of medical sciences and the Revolutionary Guards have set up similar centers with different capacities for accepting patients. For example, Iranmal convalescence, under the supervision of Iran University of Medical Sciences, provided services to 123 patients during 51 working days. Shahid Beheshti University of Medical Sciences identified three places to construct convalescent homes under its control. Due to the importance of time in this case, a closed clinic was used to build the first convalescent center with 70 beds. Also, Sorkheh Hesar and Khaqani convalescent centers were established in the crisis management sheds of the municipality, each with a capacity of 60 beds and equipped with medical supplies to complete the process of serving patients [14].
Considering the advantages of these centers, they can be used in the design and operation of temporary medical centers. According to our knowledge, there is limited information on the performance and advantages of temporary medical centers during the COVID-19 pandemic. As a result, this qualitative study aims to determine the temporary medical centers’ advantages in response to the COVID-19 pandemic.
Materials and Methods
This qualitative research in Iran employed a content analysis approach. Between March and July 2021, in-depth and semi-structured interviews were conducted with people actively involved in managing the COVID-19 pandemic. The participants included patients, experts in construction, and equipment and maintenance specialists. The participants were working in the temporary medical centers. They had a history of dealing with biological agents in the Tehran emergency health system. This group comprised combat medicine managers, non-operating defense experts, disaster reduction offices, and operation and crisis experts with at least one year of work experience in this field. The inclusion criteria were a willingness to participate in the study, effective communication with the interviewer, and informed consent. The exclusion criterion was an inability to continue with the research.
This study employed a combination of purposeful, snowball, and theoretical samplings [15]. Purposeful sampling guided the selection of the interviewees. The theoretical sampling determined the number of people, required data sources, and the study objectives. This type of sampling with rich information helps investigate and analyze the nature and dimensions of the phenomenon better [16]. The snowball sampling was used to identify experts other than those initially participating in the study. Therefore, by preparing a sampling matrix, 22 experts were selected with maximum variation, considering criteria such as work experience, age, gender, and education level. Three patients hospitalized in temporary medical centers were also included in the study.
During the interview, the researcher first introduced herself, briefly explained the objectives and significance of the study, and assured the participants about the confidentiality of their personal information. Ethical considerations were observed throughout the study, and informed consent was obtained from the participants for entering the analysis and recording of interviews. Face-to-face and semi-structured interviews were conducted with the participants in a secure environment, lasting 60 to 90 minutes and continuing until data saturation was achieved. The interviews concluded when the interviewees felt tired; answering the questions was not compulsory.
The interview questions were expanded, revised, and formulated after reviewing the literature, conducting 3 preliminary interviews (pre-test to confirm the reliability of the questions), and holding three meetings with the research team. The primary questions were asked at the beginning of the interview, and the additional questions were posed according to the participants’ responses. The interviews were transcribed verbatim at the earliest opportunity, and the conventional content analysis method proposed by Graneheim and Lundman was used to analyze the data. Coding and analyzing the data were done simultaneously after reading the interviews several times and immersing in the contents facilitated by MAXQDA software. In this way, the words and key phrases were specified and labeled as descriptive codes (examples). Subsequently, the initial codes were revised and labeled as analytical codes through higher-level abstraction. After modification, they were defined as interpretive codes (themes) [17, 18]. Then, the codes were categorized into different classes based on their similarities and differences [19].
Data trustworthiness
The quality of results was confirmed against the Guba and Lincoln criteria [20]. To increase the study’s credibility, the researchers observed the principle of diversity in sampling. At the end of each interview, the interviewer’s general understanding of the subject’s statements was briefly expressed and approved by the subject. Also, after completing the coding process and data analysis, a table of themes, subthemes, and codes, along with the participants’ quotes, was presented to 6 participants for confirmation and approval. To obtain confirmability, the researchers sent the result of data analysis along with the findings to 4 top researchers in the field of qualitative research and 5 experts and managers of temporary health centers. The necessary corrections were made according to their comments while maintaining the authenticity of the results and data. Raw data and all notes were kept for revisions at a later time. All available team members were involved in the analysis and coding process to increase the dependability. They were encouraged to express their opinions in the meetings held with them. In the end, the names of the themes and subthemes were finalized with the approval of the research team. To increase the transferability, a complete description of the entire research process was provided, the participants’ quotes were presented, and the study findings were sent to 5 people who met the inclusion criteria but did not participate for confirmation.
3. Results
Most study participants were male, had a PhD, and were specialized in health management. Three patients hospitalized in temporary health centers had high school diploma or Bachelor’s degree (Table 1).
According to the results, despite the problems and limitations, temporary medical centers have many advantages and positive functions, which emphasize the importance of these centers in policies and programs. Multiple advantages and functions of temporary medical centers can be classified into 8 subthemes (Table 2).
Multiple advantages and functions
Resource management, including human resources, is one of the most important components of preparation and performance in response to the COVID-19 pandemic. Establishing temporary medical centers significantly reduces disasters’ negative impact and saves human lives. These centers can act as protectors in times of crisis, and due to limitations in human resources and the urgency of intervention, they can provide much-needed care and medical interventions to the public. Although these centers encounter many challenges and constraints, they possess several advantages and positive functions, which have been classified into 8 subthemes in this study: patient-centered care, quick performance and response, helping the health system, preventing the burnout of treatment staff, savings the costs, justice and equality, leveling and providing classified services at different levels, and timely patient transfer.
Patient-centered care
One of the most important issues in temporary medical centers is the patient-centered care. Because these centers are built with specific goals, they show the highest level of effectiveness in times of crisis with the least paperwork and administrative bureaucracy. In normal conditions, according to the management of resources, regulations, and standards, a lot of time is spent on paperwork and other bureaucratic procedures in hospitals. However, this time is minimized in temporary medical centers, and the focus is on providing essential care. The main goal of these centers is to mitigate problems, treat patients, and control the atmosphere by using all-around support. Although there are no standard and listed structures in many cases, patients’ complaints and feedback are considered. Compliance with ethical principles is a basic criterion in establishing and operating these centers. In interviews with experts, control of the atmosphere in the region, treatment of patients, standardization of procedures and policies, compliance with ethical principles, review of error reports, psychosocial support of patients, follow-up of patient’s complaints, and appropriate feedback, accountability to society, patient safety and the importance of people’s lives were the most important factors mentioned.
“When we took action to control the Coronavirus, the situation completely changed, and we felt that a kind of peace returned to the society because people saw that healthcare workers are trying to provide the necessary care to people as quickly as possible” (Interviewee No. 3).
“You see, all measures taken in these centers are for public health and based on ethical philosophy. They were trying to get people treated quickly by providing patient-centered care and treatment while observing ethical principles. They were trying to provide patients the highest level of treatment” (Interviewee No. 9).
Quick performance and response
One of the most important features of temporary medical centers is the quick performance and response of these centers to crises. Considering that these centers are set up in response to crises, immediate reaction should be one of the essential characteristics of these centers. These centers should have the highest and best possible answer to the crisis immediately. A quick and correct response requires strong planning and management, though sometimes this quick response may lead to mistakes. However, according to their mission, these centers try to minimize errors. Usually, these centers are opened when society needs quick action and response. They also help other institutions and departments involved in the incident. The incident-oriented response, attention to the type of disaster and related needs, provision of strong support during the event, prevention of overload to conventional hospitals, quick structuring, prompt access, purposefulness, innovative methods of work and activity, referral to the reference laboratory in cases of need, multiple monitoring, and immediate referral were the most important factors mentioned by the interviewees.
“For example, temporary medical centers can be partly or completely relocated. They can also be set up in a building with a very different use. The mobility and speed of actions when setting up medical centers and even moving and deploying employees in the required places are also high in these centers” (Interviewee No. 17).
Helping the health system
Events and crises create many challenges for the health system in any country. Depending on the type of event, the health system bears the greatest responsibility. Typically, the health systems could not deal with these crises in most cases because of their facilities and human resources limitations. On the other hand, the suddenness of the crisis and its unknown consequences require an immediate and accurate response, which is practically impossible in the first hours of the crisis. If the health system is not supported, it may disintegrate under enormous pressure. Temporary medical centers provide the highest level of help to the health system because they take over part of the duties of hospitals and transfer only urgent and emergency cases to hospitals using a screening system. Among the most important codes extracted in this study, we can refer to the provision of basic clinical care, infection control, training of emergency measures, implementation of infection control measures, meeting basic medical needs, isolation, information provision, control of the atmosphere, and reduction of service delivery time.
“Sometimes, the establishment and operation of a center take away a large amount of pressure from hospitals and help them to treat acute cases more carefully. These centers are helpful as they provide primary clinical care and correct information” (Interviewee No. 6).
Preventing the burnout of treatment staff
Job burnout has been one of the main problems of medical staff in recent years. Many studies have explored the burnout of medical staff and showed a high burnout among healthcare workers. Job burnout may surge in a crisis like a biological event due to its social and psychological consequences, which leads to other problems. One of the solutions to the problem of burnout in medical staff and to reduce the work pressure is the establishment of temporary hospitals and medical centers and the use of trained volunteers. Coordination and management of employees, appropriate management of the supplies, reduction of workload in hospital personnel, interaction with the hospital, sharing of care and treatment duties, support of employees and their families, and establishment of the rest and welfare centers for treatment staff were the most important codes extracted from the participants’ statements. According to the instructions of these centers, the interaction between treatment staff and even between personnel and management teams should be continued, and the employees should be comfortable in expressing their opinions and wishes. This simple act helps treatment staff to keep their morale and vitality. This measure can also minimize the job burnout of treatment staff.
“We saw how happy the hospital staff were about establishing these centers, and sometimes they personally came and thanked us and said that if it wasn’t for you, we couldn’t have been able to handle the public demand, and maybe we would have given up” (Interviewee No. 4).
Saving the costs
Heavy medical expenses are one of the main problems that should be considered in times of crisis. Due to the unknown nature of diseases and events, many diagnostic and treatment measures should be taken at the outset. Suppose appropriate and practical steps are not thought out for times of crisis, and we do not have relevant policies for these times. In that case, we will incur high social and economic costs, and the expected results will be minimized. Setting up temporary medical centers during the COVID-19 pandemic is an appropriate policy, which greatly reduces unnecessary costs and helps the health system cope with public demand in times of crisis. In addition to the macro level, at the community level, these centers help individuals and families receive the same treatments and care they would receive in normal hospitals at a much lower cost and in a shorter time.
“Well, one of the duties of public centers is to respond to crises or disasters. However, it is not always possible to respond to these crises easily because the income does not match the expenses, and it is not cost-effective for private centers to have dual-purpose equipment. These centers have a plan but are less extensive than public hospitals. Hospitals also have high expenses during a crisis, so these centers help save the costs” (Interviewee No. 10).
“If you compare the cost of treatment in these centers and normal hospitals, you will see a big difference, so they are very helpful. People immediately go to these centers after getting infected because they have easy access. People either get treatment or at least information on where to go” (Interviewee No. 1).
Justice and equality
Justice and equality are two key and frequent concepts seen in the literature of all fields in recent years. Despite the importance of these two concepts, the difference between them is still debatable. Justice in health means treating all people based on their needs and conditions in such a way that makes even the situation. However, equality refers to equal treatment for everyone regardless of the situation. In times of crisis and events, both concepts are important. Under normal conditions, people with better financial status use more and better facilities and can get admitted to hospitals with more equipment. Still, people with lower social and economic status may be unable to use the necessary facilities and often do not get what they need. However, this disparity is not acceptable in a crisis. These centers provide equal services to everyone in need, regardless of their social and economic status. This action is equivalent to justice in health care access for all society members. In the biomedical field, having access to and benefitting from quality services, and in the social field, offering financial support for service users, especially the needy and people with low incomes, are the goals of justice in the healthcare system. Access to services should be easy, team-based, continuous, integrated with appropriate technology, and available for all age and gender groups. Health systems should ensure that all people can access health services in their nearest residence, benefit from these services at times of need, and are financially protected.
However, at the time of biological events, hospitals may intentionally ignore justice and equality in access and service delivery and provide unequal services to people in a targeted manner, considering their facilities and the situation. Therefore, justice and equality can be specific to these centers; in other words, temporary medical centers provide services to all patients needing treatment regardless of their differences. Among the codes extracted in this study were immediate admission of all potential patients, easy access, no attention to personality traits in admission, low cost, lack of attention to social characteristics, no discrimination, quick treatment, detection of vulnerabilities, and holistic approach.
“... Now, a person with money can easily go to a private hospital with the best facilities and get faster and better treatment, but what about the poor people in the city or countryside? They sometimes do not have access to even minimum care, which is injustice. This condition means inequality in access, inability to purchase services, and unavailability of health services. However, temporary medical centers can provide basic facilities even in low-income places, and we can say that they look at everyone equally. For them, everyone’s health is important, not the health of a few...” (Interviewee No. 13).
Leveling and proving classified services at different levels
One of the temporary medical centers’ main advantages and functions is the possibility of leveling services. Hospitals and conventional health centers are set up with a fixed purpose; changing this purpose is impossible or requires a lot of money. Temporary medical centers can operate at different levels of service delivery based on different situations and needs in times of crisis. As primary screening centers, they can remove the burden of hospitals. They also play a comparable role with hospitals and provide all the necessary services to needy people. After receiving the main services in the hospital, people can receive post-hospital services in these centers. These services facilitate the continuation of the treatment process as well as rehabilitation. It should be noted that in crises and biological incidents, these centers mostly play a prehospital role. By screening and providing primary services and referrals, they play a significant role in helping hospitals and the healthcare system. Furthermore, health promotion, prevention, treatment, and rehabilitation services are integrated into these centers as comprehensive services delivered to people who need them. Different levels of service provision, post-hospital services, second-level services, primary services, grouping of physicians, service provision and division of workforces according to services, need-based services, minimum service level, want level (what we want and like to be better), perfect and ideal levels, the possibility of developing and expanding services, and changing the use of centers and organizations were among the extracted codes related to this subtheme.
“Most of the post-hospital services are provided here. Prehospital services can also be considered as triage. If patients are considered outpatients, they will receive medication; if they are seriously ill, they will be sent to the designated hospitals. Specialists are constantly present in prehospital centers, but specialists can be on-call in post-hospital centers. This system is like a chain of service provision. The patient’s file is created in the outpatient clinic, and if he needs inpatient care, he will be referred to the hospital” (Interviewee No. 14).
“If we want to level the services based on needs, one of these levels is the minimum level (must level), which means that we cannot ignore it. One level higher is the want level, which indicates what we want and like to be better. Another level is the perfect and ideal level, which depends on the conditions and facilities and at which level you want to develop this platform”(Interviewee No. 17).
Timely patient transfers
The last subtheme related to the advantages and functions of temporary medical centers is swift patient transfer. This subtheme is considered one of the basic components of service provision in the health system, which can vary in different conditions. Access to medical centers and service delivery is one of the most influential topics in this field. An immediate transfer and providing appropriate and timely service refer to simple access to the desired center and patients’ transfer to them as soon as possible. Since the temporary medical centers are established in a targeted manner and specific places, two points should be considered in setting up these centers. First, they should be set up in areas with the least access to health and medical centers. Second, they should be set up in places with easy and quick access to other centers and hospitals. In other words, these centers act as a bridge between people needing treatment and hospitals. Patient transfer system; integrated transport protocols; a comprehensive and sustainable approach for flexibility, screening, and rapid transfer of patients to specialized centers; and having a strategy to improve performance, increase accessibility, reduce time, and help the operation of health care centers were the most important codes extracted about this sub-theme.
“... Access to care should be provided for people in all places, and there should be no need to transfer patients from one place to another because this drawback is the basis for the transmission of virus from one place to another” (Interviewee No. 12).
“The capacity created in the outpatient department to work effectively is important regarding access and not requiring patient transfer to other places. So, these centers should be set up in different parts of the city and be able to manage patients without transferring unnecessary cases to higher levels of services” (Interviewee No. 16).
Discussion
Throughout human history, infectious diseases such as plague, SARS, COVID-19, and influenza have greatly threatened human health, leaving millions dead. However, humans have dealt with these diseases by isolating infected people and breaking the cycle of infection [21-23]. Due to the inadequate resources in some countries, they have decided to build temporary health centers by converting different venues and hotels into temporary medical centers. This study aimed to highlight the advantages and performance of temporary medical centers in response to the COVID-19 pandemic.
We found that temporary medical centers have many advantages, such as immediate admission of all potential patients and easy access to health services regardless of personality traits. These centers have certain characteristics, such as low treatment costs, not considering social characteristics, lack of discrimination, and fast treatment. In general, establishing temporary medical centers effectively controls infectious diseases when the resources are scarce. By admitting patients with mild symptoms, temporary medical centers reduce the transmission of the virus and, as a result, the number of new cases. The experiences of China in fighting the COVID-19 pandemic indicate that temporary centers should provide people with easy access to health care [3, 24]. Although previous studies have shown that temporary centers should be close to key organizations, this proximity may increase disease transmission [25].
Temporary medical centers with specific standards, procedures, and policies control infection and treat patients in areas with high disease prevalence. By complying with moral principles and providing psychological and therapeutic support, these centers can respond to the needs of society in times of crisis. In line with the present study’s findings, previous studies have also shown that temporary hospitals should accept patients with mild symptoms, ensure their safety, and pay attention to their social and emotional needs [3]. The use of volunteers or untrained staff affects the quality of services. Experiences of temporary centers in China indicate that the employees and workforce should be selected in a way that guarantees the safety, quality, and efficiency of care services [26].
Other relevant studies have referred to factors such as monitoring of nurses, standardization of equipment, disinfection of the environment, reducing patients’ fear and anxiety, and strengthening emotional interaction between patients and physicians as the necessity of running temporary medical centers [24, 27]. Some studies have referred to developing protocols, instructions, and processes in response to COVID-19 in these centers [1, 28]. It is necessary to develop clinical protocols to manage patients in critical conditions, evaluate new symptoms, and manage staff. These protocols have been adopted from the standard care of the hospital system, the consensus of experts, and recommendations of disease control and prevention centers [11].
The present study showed that after being quickly established in a targeted manner, temporary treatment centers could increase the chances of patients’ recovery, provide primary clinical care and screening, help identify severe cases in the early stages, and refer them to the hospital. Moreover, by providing strong support, meeting patients’ basic medical needs, isolating infected cases, and conducting necessary tests and monitoring, these canters can reduce the number of hospital admissions and visits to healthcare centers. They can also reduce the workload of hospital staff by providing emergency measures, implementing infection control policies, sharing information, controlling the atmosphere, reducing operation time, and using low-cost equipment with low maintenance costs, which reduces treatment time and costs. Previous studies have shown that the number of physicians can be reduced in temporary treatment centers, as they mostly treat people with mild symptoms. By improving management efficiency, they can reduce costs and the need for human resources [7, 29]. However, due to these centers’ lack of specialized equipment, they should identify critically ill patients and refer them to hospitals as soon as possible [30].
Also, underlying diseases of elderly patients were managed in these centers, and counseling was offered to all patients if they wished. Several activities were also considered to relax the patients and improve the relationship between the patient and the doctor [26].
Previous studies have underscored understanding and respecting the customs of patients and local staff in these centers. This measure would promote communication and coordination between staff with different cultural backgrounds and provide the best patient care [31]. Cultural norms, special customs, non-acceptance of instructions, and mistrust of people in these centers can affect their operation and success [32]. The fear of families and health workers being exposed to the disease is also one obstacle for temporary medical centers.
Previous studies have considered it necessary to fully understand and respect the customs of patients and local staff in these centers, which would promote communication and coordination between staff with different cultural backgrounds and provide the best patient care [33].
Similar to our results, previous studies categorized the outcomes of establishing temporary medical centers. The first outcome is accelerating the diagnosis and increasing the recovered cases that showed initial effects on controlling the COVID-19 pandemic. The second outcome refers to a rapid increase in discharged patients, admissions, and treatment in temporary centers. This outcome also shows the control effects of the centers. In the third outcome, the COVID-19 pandemic showed a significant improvement. The last group of these centers achieved regular success in controlling the pandemic and played an important role in defeating the COVID-19 pandemic [34].
Among the advantages of temporary medical centers identified in the present study, we can refer to information management, integrated patient transport protocols and systems, and strategies to improve performance and increase accessibility. One of the most important aspects of disaster and emergency response is to ensure effective, frequent, and timely information exchange. In setting up temporary treatment centers, it is vital to pay attention to information management and discussion, so the management of these centers should be based on the information and communication management system [35, 36].
Among other benefits of temporary medical centers, we can point to the success in performing assigned tasks, coordination and management of employees, proper management and preparation of supplies, interaction with referral hospitals, the existence of support for employees and their families, the establishment of rest and welfare centers for employees, and prevention of job burnout. Previous studies on the response to biological attacks have pointed out problems related to quarantine, primary medical care, and daily management of patients. They have emphasized the importance of a quick response management system, creating a disease management team, and forming an appropriate medical structure [7]. Previous studies also considered the lack of proper planning as a major challenge of temporary medical centers [6, 36, 37].
Conclusion
The COVID-19 pandemic has led to an unprecedented health and economic crisis with profound and multifaceted consequences worldwide. Securing the operation of health centers to deal with the spread of such a highly contagious and deadly disease has been the top priority of many governments. One of the key elements to reduce the overload of care in large hospitals during peak health emergencies is the development of flexible policies for admitting many patients. These temporary centers, with specific criteria for accepting patients, ensuring their safety in care, helping to break internal transmission, and paying attention to the social and emotional needs of patients, as a rapid response mechanism, can respond to the current COVID-19 pandemic as well as other epidemics in future. The result of this study can be used in managing biological emergencies in the future because it provides a clear picture of the multiple advantages and functions of temporary medical centers.
Limitations
According to the characteristics of qualitative research, the generalization of the results of this study is limited only to the study environment. Therefore, conducting similar studies in other departments is recommended. Gaining access to experts was another limitation in this study, but interviews were conducted with key stakeholders. Another limitation of this study was its coincidence simultaneity with the COVID-19 pandemic. The limited interview time due to the busy work schedule and working in management positions of some participants was also a limitation of this study.
Ethical Considerations
Compliance with ethical guidelines
The present study was approved by the Iran Army University of Medical Sciences (Code: IR.AJAUMS.REC.1400.254). To comply with the ethical principles in the research, written informed consent was obtained from the participants, and the interview time was organized with them. All participants were told about the voluntary nature of participation in the study and to withdraw from the interview at any time. The interview process and how to publish the results were also explained to the participants, and they were assured that their names would remain confidential in publishing the results.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Conceptualization, supervision and data analysis: Maryam Moradi and Simintaj Sharififar; Methodology: Maryam Moradi, Simintaj Sharififar and Armin Zareiyan; Data collection: Maryam Moradi; Funding acquisition, resources, investigation, and writing: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors thank all the participants of the interview process for giving their valuable time and cooperation. In addition, the authors would also like to extend their gratitude to anonymous reviewers for their helpful comments and suggestions.
References
- Li H, Lian H, Lin J, Chen K, Lyu Y, Chen Y. Mobile cabin hospital compulsory quarantine for mild patients can serve as an alternative treatment for COVID-19: The Chinese experience. American Journal of Translational Research. 2022; 14(5):3132-42. [DOI:10.1101/2020.07.26.20162206]
- Sharififar S, Hamidi Farahani R, Khoshvaghti A, Ahmadi Marzaleh M. Designing and validation of the nurses' preparedness to response to COVID-19 questionnaire in Iran. Disaster Medicine and Public Health Preparedness. 2021; 1-7. [DOI:10.1017/dmp.2021.233] [PMID] [PMCID]
- Chen S, Zhang Z, Yang J, Wang J, Zhai X, Bärnighausen T, et al. Fangcang shelter hospitals: A novel concept for responding to public health emergencies. The Lancet. 2020; 395(10232):1305-14. [DOI:10.1016/S0140-6736(20)30744-3] [PMID]
- Shammi M, Bodrud-Doza M, Towfiqul Islam ARM, Rahman MM. COVID-19 pandemic, socioeconomic crisis and human stress in resource-limited settings: A case from Bangladesh. Heliyon. 2020; 6(5):e04063. [DOI:10.1016/j.heliyon.2020.e04063] [PMID] [PMCID]
- Barrett K, Khan YA, Mac S, Ximenes R, Naimark DMJ, Sander B. Estimation of COVID-19-induced depletion of hospital resources in Ontario, Canada. Canadian Medical Association Journal. 2020; 192(24):E640-6. [DOI:10.1503/cmaj.200715] [PMID] [PMCID]
- Aminizadeh M, Farrokhi M, Ebadi A, Masoumi GR, Kolivand P, Khankeh HR. Hospital management preparedness tools in biological events: A scoping review. Journal of Education and Health Promotion. 2019; 8:234. [PMID] [PMCID]
- Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel Coronavirus-infected pneumonia in Wuhan, China. JAMA. 2020; 323(11):1061-9. [DOI:10.1001/jama.2020.1585] [PMID] [PMCID]
- Castro Delgado R, Pérez Quesada P, Pintado García E, Marañón Zabalza I, Vallina-Victorero Vázquez M, Escribano Balín R. Alternate care sites for COVID-19 patients: Experience from the H144 Hospital of the health service of the principality of asturias, Spain. Prehospital and Disaster Medicine. 2021; 36(6):774-81. [DOI:10.1017/S1049023X2100110] [PMID] [PMCID]
- Shu L, Ji N, Chen X, Feng G. Ark of life and hope: the role of the Cabin hospital in facing COVID-19. Journal of Hospital Infection. 2020; 105(2),351-2. [DOI:10.1016/j.jhin.2020.03.032] [PMID] [PMCID]
- Adams A. Borrowed buildings: Canada's temporary hospitals during World War I. Canadian Bulletin of Medical History. 1999; 16(1):25-48. [DOI:10.3138/cbmh.16.1.25] [PMID]
- Naganathan S, Meehan-Coussee K, Pasichow S, Rybasack-Smith H, Binder W, Beaudoin F, et al. From concerts to COVID: Transforming the RI Convention Center into an Alternate Hospital Site in under a month. Rhode Island Medical Journal. 2020; 103(6):8-13. [PMID]
- Shi F, Li H, Liu R, Liu Y, Liu X, Wen H, et al. Emergency preparedness and management of mobile Cabin hospitals in China during the COVID-19 pandemic. Frontiers in Public Health. 2022; 9:763723. [DOI:10.3389/fpubh.2021.763723] [PMID] [PMCID]
- Yuan Y, Qiu T, Wang T, Zhou J, Ma Y, Liu X, et al. The application of temporary ark hospitals in controlling COVID-19 spread: The experiences of one Temporary Ark Hospital, Wuhan, China. Journal of Medical Virology. 2020; 92(10):2019-26. [DOI:10.1002/jmv.25947] [PMID] [PMCID]
- Shamsi Gamchi N, Beladian SE, Torabi S A, Mohammadnazari Z. [Establishment of Coronavirus post-hospital recovery sites by Shahid Beheshti University of Medical Sciences: Action report and logistical analysis (Persian)]. Disaster Prevention and Management Knowledge. 2020; 10(3):264-76. [Link]
- Campbell S, Greenwood M, Prior S, Shearer T, Walkem K, Young S, et al. Purposive sampling: Complex or simple? Research case examples. Journal of research in Nursing. 2020; 25(8):652-61. [DOI:10.1177/1744987120927206] [PMID] [PMCID]
- Speziale HS, Streubert HJ, Carpenter DR. Qualitative research in nursing: Advancing the humanistic imperative. China: Lippincott Williams & Wilkins; 2011. [Link].
- Forman J, Damschroder L. Qualitative content analysis. In: Jacoby L, Siminoff LA, editors. Empirical methods for bioethics: A primer. Leeds: Emerald Group Publishing Limited; 2007. [DOI:10.1016/S1479-3709(07)11003-7]
- Holley RP. Applications of social research methods to questions in information and library science (review). Portal: Libraries and the Academy. 2009; 9(4):517-8. [DOI:10.1353/pla.0.0081]
- Tesch R. Qualitative research: Analysis types and software. London: Routledge; 2013. [DOI:10.4324/9781315067339]
- Lincoln YS, Guba EG. But is it rigorous? Trustworthiness and authenticity in naturalistic evaluation. New Directions for Program Evaluation. 1986; 1986(30):73-84. [DOI:10.1002/ev.1427]
- Wever PC, van Bergen L. Death from 1918 pandemic influenza during the First World War: A perspective from personal and anecdotal evidence. Influenza and Other Respiratory Viruses. 2014; 8(5):538-46. [DOI:10.1111/irv.12267] [PMID] [PMCID]
- Paules CI, Marston HD, Fauci AS. Coronavirus infections-More than just the common cold. JAMA. 2020; 323(8):707-8. [DOI:10.1001/jama.2020.0757] [PMID]
- Lai CC, Shih TP, Ko WC, Tang HJ, Hsueh PR. Severe Acute Respiratory syndrome Coronavirus 2 (SARS-CoV-2) and Coronavirus disease-2019 (COVID-19): The epidemic and the challenges. International Journal of Antimicrobial Agents. 2020; 55(3):105924. [DOI:10.1016/j.ijantimicag.2020.105924] [PMID] [PMCID]
- Chen X, Chen H, Chen YG, Yao JG. Cabin hospital for COVID-19 patients: Attention should be paid to hospital infection prevention, humanistic care, and privacy protection. The Kaohsiung Journal of Medical Sciences. 2021; 37(8):739-40. [DOI:10.1002/kjm2.12382] [PMID] [PMCID]
- Fang D, Pan S, Li Z, Yuan T, Jiang B, Gan D, et al. Large-scale public venues as medical emergency sites in disasters: Lessons from COVID-19 and the use of Fangcang shelter hospitals in Wuhan, China. BMJ Global Health. 2020; 5(6):e002815. [DOI:10.1136/bmjgh-2020-002815] [PMID] [PMCID]
- Zhu W, Wang Y, Xiao K, Zhang H, Tian Y, Clifford SP, et al. Establishing and managing a temporary Coronavirus disease 2019 Specialty Hospital in Wuhan, China. Anesthesiology. 2020; 132(6):1339-45. [DOI:10.1097/ALN.0000000000003299] [PMID] [PMCID]
- Xiao Y, Torok ME. Taking the right measures to control COVID-19. The Lancet Infectious Diseases. 2020; 20(5):523-4. [DOI:10.1016/S1473-3099(20)30152-3] [PMID]
- Candel FJ, Canora J, Zapatero A, Barba R, González Del Castillo J, García-Casasola G, et al. Temporary hospitals in times of the COVID pandemic: An example and a practical view. Revista Española de Quimioterapia. 2021; 34(4):280-8. [DOI:10.37201/req/041.2021] [PMID] [PMCID]
- Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. Clinical features of patients infected with 2019 novel Coronavirus in Wuhan, China. The Lancet. 2020; 395(10223):497-506. [DOI:10.1016/S0140-6736(20)30183-5] [PMID]
- Dowlati M, Seyedin H, Moslehi S. Hospital preparedness measures for biological hazards: A systematic review and meta-synthesis. Disaster Medicine and Public Health Preparedness. 2021; 15(6):790-803. [DOI:10.1017/dmp.2020.132] [PMID]
- Liu L, Yin H, Liu D. Zero health worker infection: Experiences from the China Ebola Treatment Unit during the Ebola epidemic in Liberia. Disaster Medicine and Public Health Preparedness. 2017; 11(2):262-6. [DOI:10.1017/dmp.2016.103] [PMID]
- von Strauss E, Paillard-Borg S, Holmgren J, Saaristo P. Global nursing in an Ebola viral haemorrhagic fever outbreak: Before, during and after deployment. Global Health Action. 2017; 10(1):1371427. [DOI:10.1080/16549716.2017.1371427] [PMID] [PMCID]
- Zhang Y, Shi L, Cao Y, Chen H, Wang X, Sun G. Wuhan mobile cabin hospital: A critical health policy at a critical time in China. Medicine (Baltimore). 2021; 100(3):e24077. [DOI:10.1097/MD.0000000000024077] [PMID] [PMCID]
- Tadavarthy SN, Finnegan K, Bernatowicz G, Lowe E, Coffin SE, Manning M. Developing and implementing an infection prevention and control program for a COVID-19 alternative care site in Philadelphia, PA. American Journal of Infection Control. 2021; 49(1):77-81. [DOI:10.1016/j.ajic.2020.07.006] [PMID] [PMCID]
- Wurmb T, Scholtes K, Kolibay F, Schorscher N, Ertl G, Ernestus RI, et al. Hospital preparedness for mass critical care during SARS-CoV-2 pandemic. Critical Care (London, England). 2020; 24(1):386. [DOI:10.1186/s13054-020-03104-030] [PMID] [PMCID]
- Montejano-Castillo M, Moreno-Villanueva M. Hospitals safe from disasters: A glimpse into the Mexican coastal zones. International Journal of Safety and Security Engineerings. 2018; 8(2):329-41. [DOI:10.2495/SAFE-V8-N2-329-341]
- Azarmi S, Pishgooie AH, Sharififar S, Khankeh HR, Ziya HS. Disaster risk management challenges in military hospitals: A qualitative study. Journal of Education and Health Promotion. 2022; 11:167. [DOI:10.4103/jehp.jehp_690_21] [PMID] [PMCID]
Type of article: Research |
Subject:
Qualitative
Received: 2023/04/12 | Accepted: 2023/07/2 | Published: 2023/09/11
Received: 2023/04/12 | Accepted: 2023/07/2 | Published: 2023/09/11
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |