Volume 9, Issue 3 (Spring 2024)
Health in Emergencies and Disasters Quarterly 2024, 9(3): 211-220 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Torabi M, Borhani F, Abbaszadeh A, Oshvandi K, Khazaie S, Masoumi H. Investigating the Relationship Between Moral Distress and Ethical Climate Among Emergency Medical Services Personnel. Health in Emergencies and Disasters Quarterly 2024; 9 (3) :211-220
URL: http://hdq.uswr.ac.ir/article-1-562-en.html
URL: http://hdq.uswr.ac.ir/article-1-562-en.html
Mohammad Torabi *1 

 , Fariba Borhani2
, Fariba Borhani2 

 , Abbas Abbaszadeh2
, Abbas Abbaszadeh2 

 , Khodayar Oshvandi3
, Khodayar Oshvandi3 

 , Salman Khazaie4
, Salman Khazaie4 

 , Habib Masoumi5
, Habib Masoumi5 




 , Fariba Borhani2
, Fariba Borhani2 

 , Abbas Abbaszadeh2
, Abbas Abbaszadeh2 

 , Khodayar Oshvandi3
, Khodayar Oshvandi3 

 , Salman Khazaie4
, Salman Khazaie4 

 , Habib Masoumi5
, Habib Masoumi5 


1- Chronic Diseases (Home Care) Research Centre, Malayer School of Nursing, Hamadan University of Medical Sciences, Hamadan, Iran. , mtorabi316@gmail.com
2- Medical Ethics and Law Research Center, Shahid Beheshti University of Medical Sciences, Tehran, Iran.
3- Mother and Child Care Research Center, Faculty of Nursing and Midwifery, Hamadan University of Medical Sciences, Hamadan, Iran.
4- Research Center for Health Sciences, Hamadan University of Medical Sciences, Hamadan, Iran.
5- Disaster and Emergency Medical Management Center, Hamadan University of Medical Sciences, Hamadan, Iran.
2- Medical Ethics and Law Research Center, Shahid Beheshti University of Medical Sciences, Tehran, Iran.
3- Mother and Child Care Research Center, Faculty of Nursing and Midwifery, Hamadan University of Medical Sciences, Hamadan, Iran.
4- Research Center for Health Sciences, Hamadan University of Medical Sciences, Hamadan, Iran.
5- Disaster and Emergency Medical Management Center, Hamadan University of Medical Sciences, Hamadan, Iran.
Full-Text [PDF 529 kb]
(1880 Downloads)
| Abstract (HTML) (3532 Views)
Full-Text: (879 Views)
Introduction
Emergency department personnel practice is in environments that are unpredictable and have limited decision time and high workload in nature [1]. Emergency medical services (EMS) is the first level of pre-hospital emergency medical care that provides timely care to victims of sudden and life-threatening accidents on the scene [2]. EMS personnel in Iran work in urban and road bases in pairs and often in 24-h shifts. As soon as they receive a message from the center operators, they go to the accident scene and after consulting with the medical director, perform medical procedures and transport the patient(s) to the hospital [3]. Due to the complex job nature of EMS personnel, dealing with situations that require ethical decision-making is inevitable [4]. EMS personnel are often exposed to stressful and challenging events, such as unpredictable situations, irrational requests of relatives, workplace violence, time pressure, patient privacy and confidentiality, and harrowing scenes [5, 6]. Moral distress is one of the consequences of facing such situations [7]. The concept of moral distress was originally defined by Jameton (1984) as knowing the right thing, yet institutional constraints make it impossible to pursue the right course [8]. This issue puts a lot of stress on the person. Also, moral distress is defined by the American Association of Critical-Care Nurses (AACN) in its public policy position statement as follows: “Moral distress occurs when one is morally aware of the right course of action but is unable to act upon it, and one acts in a manner contrary to their personal and professional values, which undermines their integrity and authenticity [9]”. According to studies, moral distress in healthcare professionals is derived from different factors, including the lack of resources, political structures in healthcare [10], unnecessary medical care, poor communication, family unreasonable requests [6], confidentiality, and privacy [11], and the end of life care. Evidence suggests that moral distress has consequences that include various psychological problems, such as anger, depression, frustration [12], teamwork burnout, and decreased quality of care [13]. Also, according to the findings, high levels of moral distress adversely affect work climate, job dissatisfaction [14, 15], retention, attrition, compassion fatigue, and feelings of powerlessness [16, 17]. Multiple studies in the nursing literature have shown the effect of a positive ethical climate on reducing nurses’ moral distress [17, 18].
As an integral part of the organizational culture, an ethical climate may affect nurses’ responses to ethical challenges [19]. The ethical climate is one of the mechanisms influencing employee behavior that is associated with employees’ feelings and reactions in the face of ethical issues [20]. The organization’s ethical climate reflects moral values, behavioral expectations, and the impact of ethics on members’ decisions, which provides a framework for ethical decision-making in clinical settings [21]. In other words, the ethical climate can act as a resource for employees that shapes their ethical attitudes and behaviors in the face of ethical challenges [20, 21]. It may also positively affect patient satisfaction, nursing practices, and ethical decision-making [22]. Hart’s descriptive study showed the relationship between a negative ethical climate and nurses’ decision to leave the nursing profession [23]. To date, findings suggest that an ethical climate may contribute to moral distress [19, 24], organizational commitment [25], turnover intentions, reduced job satisfaction [26], and unsafe patient care [17].
Although most studies on moral distress have been done with clinical nurses [17], it is not limited to nursing. Due to the unpredictable missions, time constraints, and locations involved, prehospital ambulance-based research has unique ethical issues than other emergency research departments [27]. According to the evidence, moral distress is influenced by personal characteristics, clinical situations, and organizational conditions [28], and ethical climate is also influenced by various factors, such as cultural, legal, and organizational regulations [29]. Also, the intensity and frequency of perceived moral distress experienced by EMS personnel and their ethical climate are affected by factors not comparable to in-hospital situations. Although several studies have been conducted on moral distress and healthcare professionals’ ethical climate [29, 30], none have been conducted on the level of moral distress and perception of ethical climate among prehospital EMS personnel in Iran. Accordingly, this study investigates the relationship between moral distress and the perceived ethical climate among EMS personnel.
The results of this study can play an essential role in better identifying factors affecting EMS employees’ moral distress. In addition, by identifying the ethical climate perceived by EMS staff, it is possible to apply the organization’s policies to improve job satisfaction and motivation, increase EMS service quality, and reduce moral distress. This study determined the relationship between ethical climate and moral distress among EMS personnel.
Materials and Methods
Study design and participants
This descriptive-correlational study was performed on EMS staff working in emergency medical centers affiliated with Hamadan University of Medical Sciences in Iran. The participants were selected via the census sampling method. A total of 136 EMS staff working in urban and road stations entered the study and completed the questionnaires. The inclusion criteria in this study included having at least a bachelor of science in nursing and medical emergency, and at least one year of working experience in EMS centers. Meanwhile, the exclusion criteria were having no history of high stress (death of relatives, family problems, and coronavirus infection in oneself or your family) in the past eight weeks.
Data collection
Before data collection, legal permits and coordination with the Medical Emergency and Accident Center authorities were obtained. Due to the wide dispersion of urban and road emergency bases and COVID-19 health protocols, the data were collected by an electronic survey. Data collection lasted from April to July 2020. The participants who had not responded within two weeks were sent an electronic reminder at weeks 2 and 6.
Study instruments
The study instrument consists of three parts as follows.
Demographic data
The demographic data included age, gender, marital status, clinical work experience, educational status, and employment status.
Moral distress instruments
Various tools are available to measure moral distress. The most common include the moral distress scale (MDS) [31], the moral distress scale-revised (MDS-R) [15], and the moral distress thermometer [32].
One of the predominant data-gathering methods in moral distress is the questionnaire, with Corley MDS [31, 33], based on Jameton’s theoretical definition. The Corley MDS is a 38-item scale that measures moral distress intensity (MDI) and moral distress frequency (MDF), ranging from 0 to 6 for each category.
The MDS-R consists of 21 items. It measures people’s perceptions of a situation based on the intensity of moral distress and the frequency of encountering it. In Iran, a psychometric evaluation of the MDS-R instrument was performed, and its reliability was confirmed using the Cronbach α [34].
The moral distress thermometer, with its 11-point scale (0-10), may be used as a screening tool for moral distress, which has less convergent validity than the moral distress instrument [32].
MDS-R is based on pre-hospital context. In this study, due to the different clinical contexts of EMS staff, some items of the MDS-R questionnaire were revised by reviewing specialized texts and qualitative studies in the field of EMS, as well as the opinions of experts in the field of EMS. Items unrelated to EMS (under pressure related to organizational costs and organ donation) were removed. Several items related to the EMS staff’s ethical distress (following orders, irrational requests from family members, caring in insecure situations, and legal conflicts) were replaced. Finally, MDS-R items for EMS reached a total of 24. MDI was scored using a 6-point Likert scale ranging from “not at all” (score 0) to “repeatedly” (score 5) and MDF with a range of “I have never experienced distress” (score 0) to “I experienced distress repeatedly” (score 5). This tool’s content validity was obtained after reviewing ten faculty members and five experts in EMS. The instrument’s reliability was measured using the Cronbach α of 0.94 and 0.91 for intensity and frequency, respectively.
Ethical climate instruments
Over time, several tools have been developed to examine ethical climate. The most common in medicine are the hospital ethical climate questionnaire (HECS) and the ethical climate questionnaire (ECQ).
Olson (1998) developed the HECS to assess nurses’ perception of the hospital’s ethical climate. The HECS consists of a 26-item survey with five subcategories (relationships with peers, patients, managers, hospital administrators, and physicians) scored on a 5-point Likert scale from 1 to 5 (1=almost never true to 5=almost always true) [35].
The ECQ was developed by Victor and Cullen (1988) and consisted of a 26-item tool that measures five types of ethical climate in an organization. In addition to instrumental, caring, independence, rules, and low and code climates, there are five ethical climates. The scoring of this questionnaire is based on the 6-point Likert scale ranging from 0=strongly disagree to 6=strongly agree [36].
A 12-item revised ethical climate questionnaire was developed for this study. According to Cullen et al. (1993), the moral distress frequency focuses on three factors of ethical criteria, namely egoism (maximizing one’s self-interests), benevolence (maximizing joint interests), and principled (adherence to universal principles) [37] to measure the agreement with each statement. The scale ranged from [1] strongly disagree to [5] strongly agree.
To examine the tool’s content validity, questionnaires were provided to experts in medical ethics. They were asked to check whether the tool statements were clear and adequately linked to the categorized dimensions. In addition, internal consistency reliability was 0.89 using the Cronbach α.
Results
Demographic characteristics
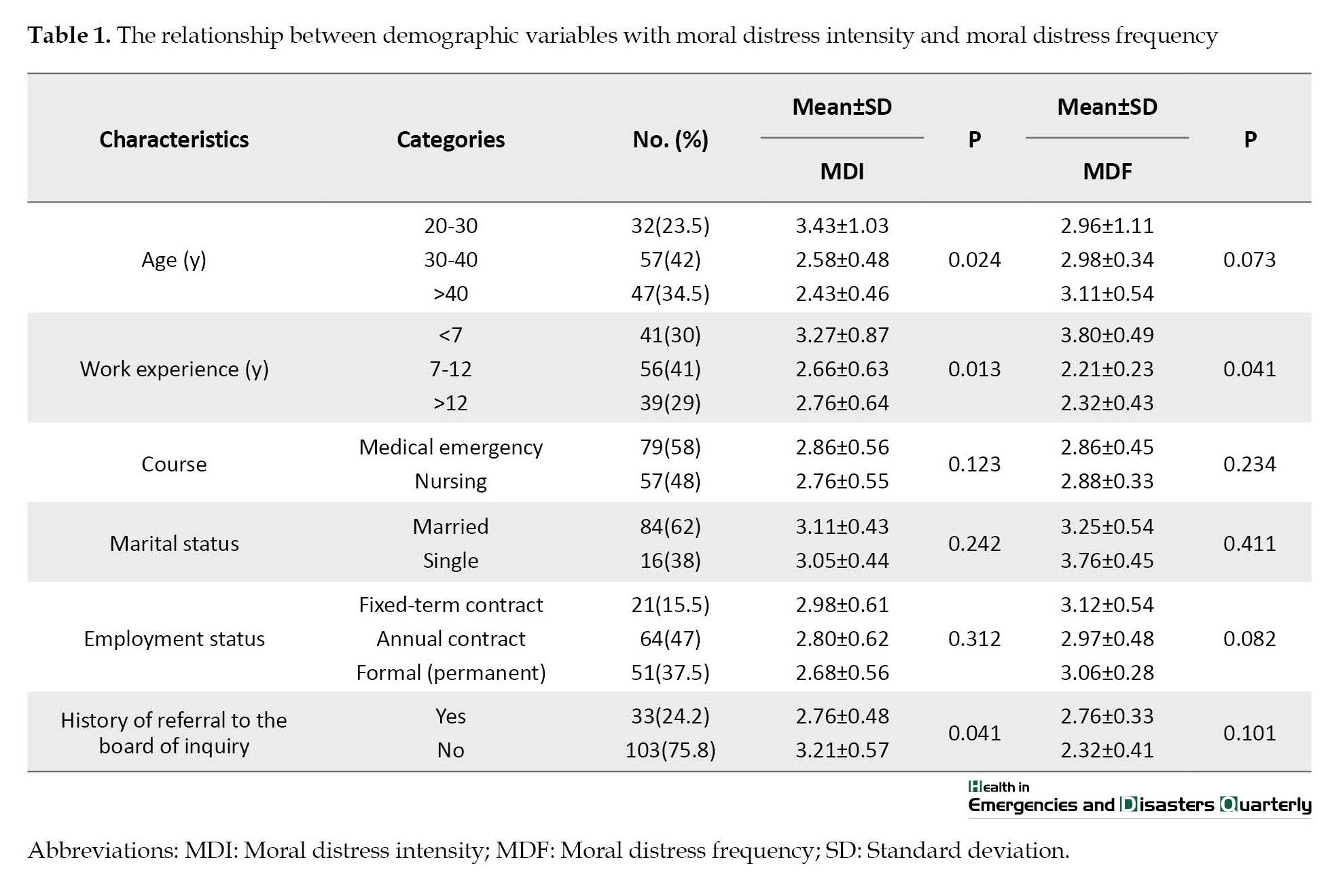
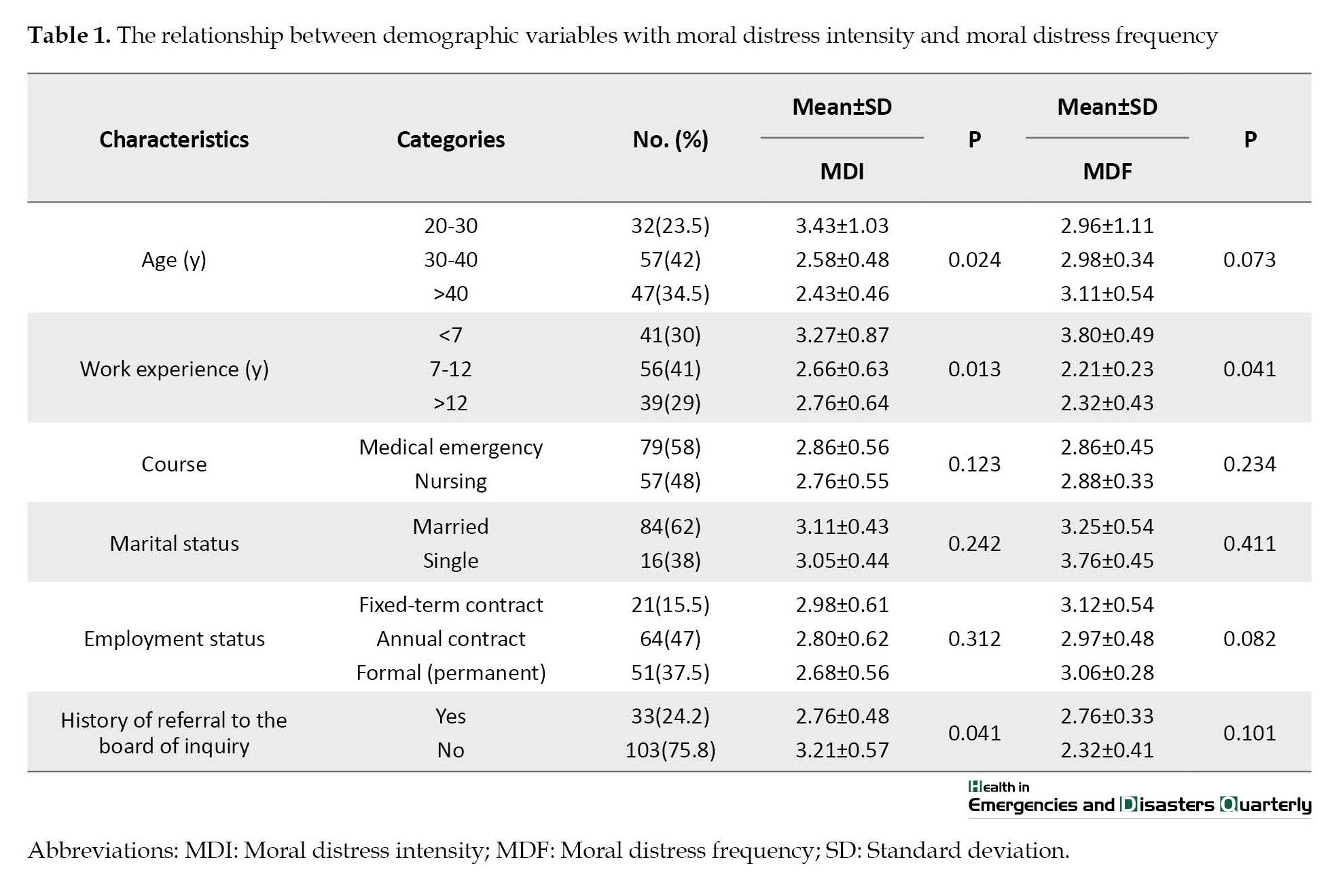
In this study, out of 154 eligible participants, 136 (88.3%) answered the questionnaire. Most of the participants were married (62%), had a bachelor’s degree in emergency medicine (58%), and had annual contract employment (47.8%). The average work experience of personnel was 10.2±3.4 years, ranging from 1 to 23 years. Their mean age was 33.4±3.54 years, ranging from 23 to 49 years. In addition, 24.2% of the personnel had a history of public complaints against them or were referred to the Board of Inquiry at least once (Table 1).
Moral distress and ethical climate
The mean MDI was 3.65±1.14 with a range of 4.83±0.62, and the mean MDF was 1.83±0.53 with a range of 3.49±0.25, which shows that the mean MDI and MDF are high and moderate, respectively. The most moral distress experienced by EMS staff was related to providing low-quality services due to high workload, having to comply with patients’ irrational requests, and caring in unsafe conditions. The mean ethical climate was moderate (2.96±1.02), with a range of 4.11±1.06. The highest score of ethical climates from the EMS staff’s perspective was related to adherence to principles, independence egoism, and benevolence, respectively. Among the questions, the highest score of ethical climates was related to the observance of professional rules and standards and the lowest score was related to the evaluation of individuals based on the organization’s interests and respecting others’ rights.
Relationship between demographic characteristics and moral distress
The results showed a significant relationship between the MDI and some personal characteristics, such as age, work experience, and having a history of referral to the Board of Inquiry (P<0.05). Accordingly, the most moral distress among employees under the age of 7 years (3.17±0.87), ages less than 28 years (3.23±1.03), and with a history of referral to the Board of Inquiry (2.14±0.57) was experienced (P<0.05). Also, moral distress in bachelor’s degree in emergency medicine (2.74±0.95) was more than in other disciplines. According to the findings, there was only a significant relationship between MDF and work experience (employees with less than seven years of experience) (P<0.05) (Table 1).
Relationship between demographic characteristics and ethical climate
The results indicated that demographic factors were not significantly related to ethical climate (P>0.05); however, the ethical climate among employees with a history of complaining or referring to the Board of Inquiry was lower than among other employees.
Relationship between moral distress intensity and moral distress frequency, and their relationship with ethical climate aspects
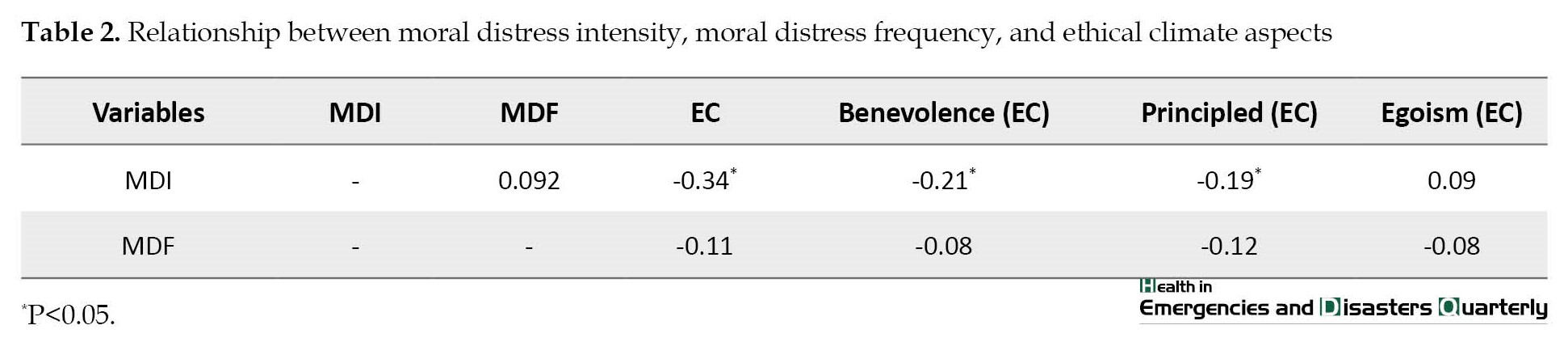
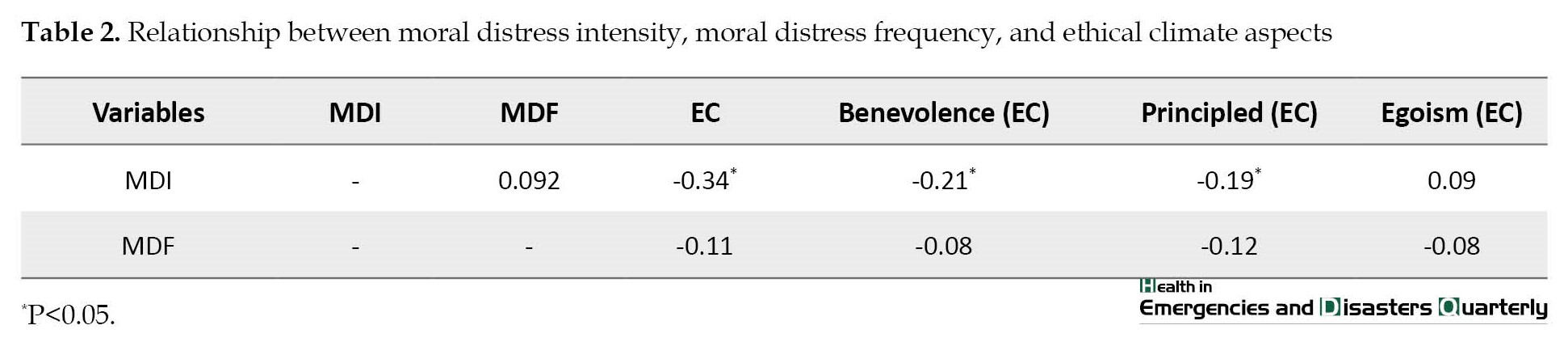
The results showed a negative and significant relationship between EC and EMS staff MDI (r=-0.34, P<0.05). However, there was no significant relationship between EC and MDF (r=-0.11, P>0.05). Based on the results, MDI was only related to the dimension of adherence to universal principles (principled). Nevertheless, MDF had no significant relationship with any of the dimensions of ethical climate (Table 2).
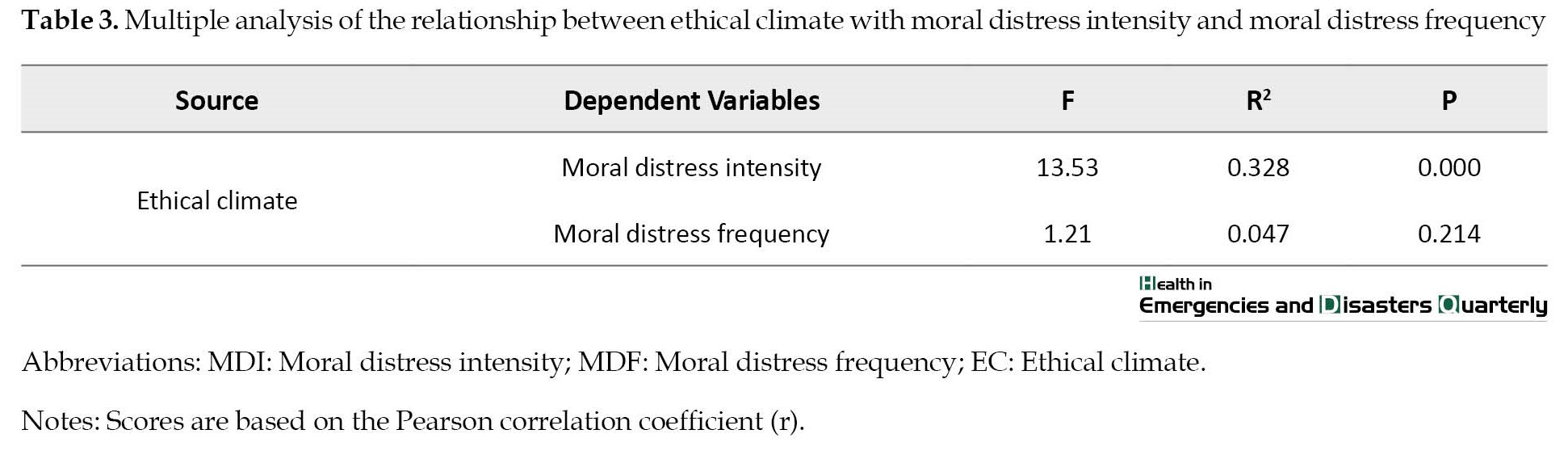
Multiple analyses of the relationship between variables simultaneously with moral distress
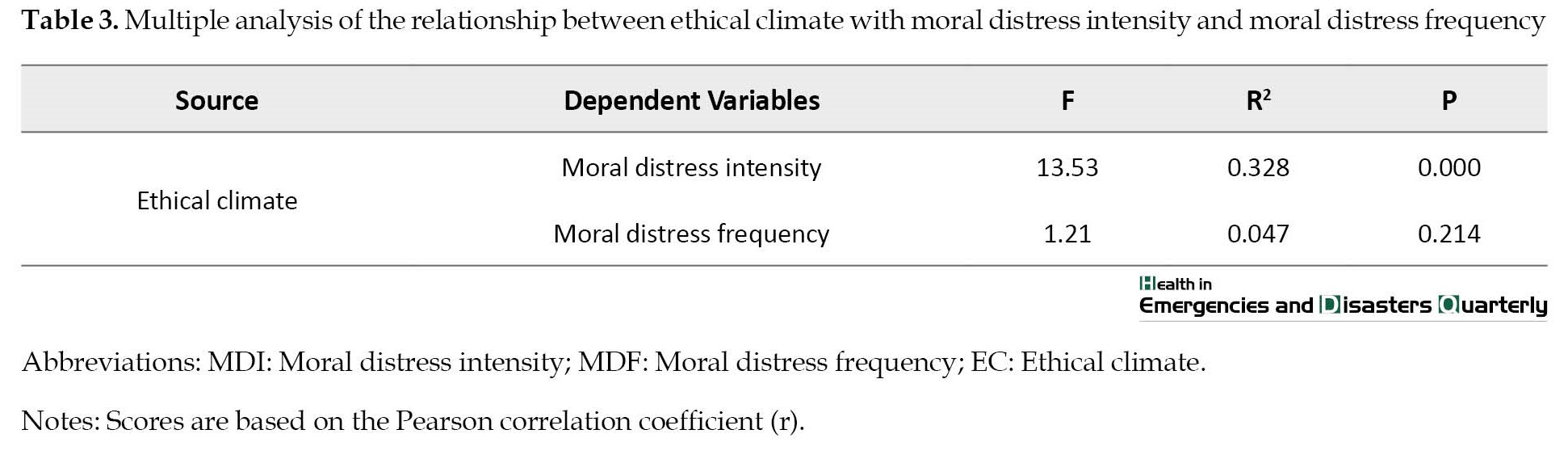
The relationship between ethical climate with the MDI and MDF using multiple linear regression analysis showed that 32.8% of the MDI is explained by ethical climate (F=13.53, R2=0.328, P<0.001) and 4.7% of the MDF is explained by ethical climate (F=1.21, R2=0.047, P>0.05) (Table 3).
At the end of the moral distress questionnaire, EMS personnel were asked to describe the most common cause of their moral distress. Some of them described moral distress in an emergency. One of them described the situation in which the injured person asked us to tell the health status of other family members in the car accident. However, it was difficult to announce family members’ deaths. Another staff member described his experiences as often asking us to perform treatment at home and not to transport their patient to the hospital due to poor financial circumstances. Some employees have pointed out that announcing bad news or family death is a common issue that causes severe distress. Other EMS staff cited challenges such as scene insecurity, inappropriate family requests, and threats to sue.
Discussion
The findings showed a significant negative relationship between MDI and the ethical climate among EMS personnel. Therefore, a positive ethical climate can reduce MDI among EMS personnel. In this regard, Lützén et al. (2010) found that ethical climate predicts and explains 33.7% of moral distress through linear regression analyses with some moral sensitivity items [18]. Some studies found a significant negative correlation between moral distress and ethical climate, indicating that a poor ethical climate is associated with higher moral distress [17, 30, 33]. Additionally, Schluter (2008) found that moral distress is inevitable in an ethical climate where the priorities are perceived to be budget and patient throughput over patient safety [21]. Janvier et al. reported that the level of moral distress among nurses depends on the work environment [38]. Additionally, Schluter et al. found that moral distress is inevitable in an ethical climate where the priorities are perceived to be budget and patient throughput over patient safety [21]. According to an ethical analysis in 2022, moral distress can undermine a physician’s ethical integrity, leading to anger, poor job satisfaction, reduced quality of care, and burnout. The analysis suggested that addressing an ethical climate could help reduce moral distress among healthcare professionals [39]. Asgari et al. and Hou et al. found that a positive ethical climate predicted lower moral distress in critical care nurses and emergency department nurses, respectively [30, 40]. Similarly, Pauly (2009) found that each aspect of ethical climate (peers, patients, managers, hospitals, and physicians) was significantly correlated with moral distress in a random sample of registered nurses [17]. However, Altaker et al. (2018) found no relationship between moral distress and ethical climate in intensive care unit nurses [41].
The results of Asgari et al. (2017), also using regression analysis, showed that among the studied variables (age, sex, work experience, marriage, job position, and ethical climate), there is only a significant relationship between ethical climate and moral distress [30]. Also, similar to our findings, several studies indicate that nurses who perceived a more positive ethical climate experienced less moral distress; therefore, EMS staff on two-person out-of-hospital missions have to make quick ethical decisions in unsafe and unpredictable situations, leading to more moral distress than in-hospital nurses. However, despite the special pre-hospital emergency conditions and the ethical climate different from hospitals, a positive ethical climate can significantly reduce EMS staff’s moral distress.
According to our study, EMS staff experienced a high level of MDI. This was often related to increased workload, unreasonable patient requests, and providing care services under unsafe conditions. Also, the mean MDF was reported to be moderate, often associated with a high workload, limited career advancement opportunities, and following superior orders. Ruston et al. (2015) indicated that employees should identify barriers to moral distress in themselves and their organization. For EMS providers, this can include the instability of the work environment, how decisions are made, interpersonal interactions, and maintaining the respect and dignity of employees within the organization [42]. Vazir et al. found that the severity of moral distress in the EMS, intensive care units, and neonatal intensive care unit staff is higher than in the other departments of internal medicine, ophthalmology, and ear, nose, and throat [43]. Jafari et al. showed that about 76% of the technicians working in EMS experienced a moderate level of moral distress [44]. In line with the present study, Salari et al. reported in a systematic review and meta-analysis that the intensity and frequency of moral distress in nurses is high [45].
Studies have also demonstrated that moral distress is prevalent among EMS staff, including emergency department nurses, due to the challenging nature of their work [46, 47]. The level of moral distress EMS staff experience depends on their role and workplace environment. ED nurses tend to experience higher moral distress than physicians, likely because they are more directly involved in patient care [40]. Staff in intensive care units and emergency departments also experience greater moral distress than those in non-critical care settings, due to the high-stakes nature of the work [40, 48].
The results of studies have shown that various factors, such as following the patients’ or families’ irrational requests, conflict of values, conflict of ethics and law, and the lack of experience are among the ethical EMS personnel challenges in their ethical decision-making [3, 4], which is consistent with some of the items of moral distress in the present study. Also, a study demonstrated that EMS personnel’s moral distress was more related to feelings of disrespect, performance in a hostile moral environment, and acting against the patient’s best interests [49]. The MDF was lower than its intensity in the present study, consistent with some studies [17, 19]. The results of the present study showed that the mean EMS personnel’s ethical climate is moderate, which is often related to adherence to principles. The results of Jalali et al. (2017) also showed that the mean ethical climate among EMS staff is at a desirable level, often related to professionalism and adherence to rules [50], consistent with the present study. According to the findings, EMS staff, like hospital nurses, seem more ethically motivated by regulations.
This study showed a significant relationship between increasing age, experience, and no complaints history or referral to the Board of Inquiry for violations, reducing moral distress intensity. In this regard, the results of some studies indicate no significant relationship between demographic characteristics and moral distress [51, 52]. Silén et al. also showed that nurses with less than six years of work experience have less moral distress than nurses with more work experience [19], which is not consistent with the findings of the present study.
The inverse relationship between work experience and history of reporting EMS staff misconduct with moral distress may be related to the impact of training classes and staff familiarity with ethical principles, standards, and rules. The experiences of EMS staff in ethical decision-making have also shown that fear of complaint, the lack of manager support, and low expertise are among the ethical decision-making barriers and create moral distress [4].
Also, according to the findings, no demographic characteristics have a significant relationship with the EMS staff’s ethical climate, consistent with some studies [17, 53].
Due to the occupational nature of medical emergencies and the cultural and organizational characteristics of prehospital emergency medical centers in Iran, it is difficult to accurately examine the relationship between the variables of ethical climate and moral distress perceived by EMS staff. Since little research has been done on ethical issues in EMS in Iran, more quantitative and qualitative research is needed to explore the factors related to moral distress and ethical climate among EMS personnel.
The findings can provide valuable information to prehospital supervisors and managers in identifying the contributing factors to moral distress from the perspective of EMS staff. The findings may also help managers plan to improve the organization’s ethical climate and ultimately increase prehospital care quality by reducing moral distress.
Conclusion
This study investigated perceived moral distress and ethical climate among EMS personnel and the associations between the MDI and MDF and different aspects of ethical climate. Accordingly, EMS personnel perceived a moderate ethical climate. The highest scores for ethical climate included adherence to principles, egoism, and benevolence, respectively. The findings showed that the mean MDI was high, while the mean MDF was moderate. The most common cause of moral distress was related to providing low-quality services due to high workload, having to comply with patients’ irrational requests, and caring in unsafe conditions. The study found a significant relationship between MDI and some personal characteristics, such as age, work experience, and having a history of referral to the Board of Inquiry. However, there was only a significant relationship between work experience and MDF. On the other hand, demographic factors did not have a significant relationship with ethical climate, except for employees with a history of complaining or referring to the research board, who had a lower ethical climate. The findings showed that a positive ethical climate could reduce EMS staff’s MDI. Therefore, to reduce moral distress and improve the ethical climate among EMS personnel, the following is recommended: Attention to the organization’s interests in evaluating employees, revision and review of employee complaints in referral to the Board of Inquiry, reduction of workload by increasing the number of emergency bases, and adjusting expectations of employees according to their circumstances.
Study limitations
Even though enough studies have been conducted to investigate the moral distress and ethical climate of nurses working in hospitals, the results reported in this study may not be generalizable to EMS personnel. Also, despite validating these questionnaires on prehospital workers, more comprehensive research with different cultural and ethnic characteristics in different countries is necessary to confirm the generalizability of the findings.
Ethical Considerations
Compliance with ethical guidelines
Ethical approval was received from the Ethics Committee of Hamadan University of Medical Sciences (Code: IR.UMSHA.REC.1398.578). Informed consent was obtained from all participants to participate in the study, and they were assured that the information would remain confidential.
Funding
This study was conducted with the support of the Vice Chancellor for Research and Technology at Hamadan University of Medical Sciences (Project No.: 9807305714).
Authors' contributions
All authors equally contributed to preparing this article.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors would like to express their gratitude to all the emergency medical staff at the Accident and Emergency Medical Center who assisted us in this study.
References
Emergency department personnel practice is in environments that are unpredictable and have limited decision time and high workload in nature [1]. Emergency medical services (EMS) is the first level of pre-hospital emergency medical care that provides timely care to victims of sudden and life-threatening accidents on the scene [2]. EMS personnel in Iran work in urban and road bases in pairs and often in 24-h shifts. As soon as they receive a message from the center operators, they go to the accident scene and after consulting with the medical director, perform medical procedures and transport the patient(s) to the hospital [3]. Due to the complex job nature of EMS personnel, dealing with situations that require ethical decision-making is inevitable [4]. EMS personnel are often exposed to stressful and challenging events, such as unpredictable situations, irrational requests of relatives, workplace violence, time pressure, patient privacy and confidentiality, and harrowing scenes [5, 6]. Moral distress is one of the consequences of facing such situations [7]. The concept of moral distress was originally defined by Jameton (1984) as knowing the right thing, yet institutional constraints make it impossible to pursue the right course [8]. This issue puts a lot of stress on the person. Also, moral distress is defined by the American Association of Critical-Care Nurses (AACN) in its public policy position statement as follows: “Moral distress occurs when one is morally aware of the right course of action but is unable to act upon it, and one acts in a manner contrary to their personal and professional values, which undermines their integrity and authenticity [9]”. According to studies, moral distress in healthcare professionals is derived from different factors, including the lack of resources, political structures in healthcare [10], unnecessary medical care, poor communication, family unreasonable requests [6], confidentiality, and privacy [11], and the end of life care. Evidence suggests that moral distress has consequences that include various psychological problems, such as anger, depression, frustration [12], teamwork burnout, and decreased quality of care [13]. Also, according to the findings, high levels of moral distress adversely affect work climate, job dissatisfaction [14, 15], retention, attrition, compassion fatigue, and feelings of powerlessness [16, 17]. Multiple studies in the nursing literature have shown the effect of a positive ethical climate on reducing nurses’ moral distress [17, 18].
As an integral part of the organizational culture, an ethical climate may affect nurses’ responses to ethical challenges [19]. The ethical climate is one of the mechanisms influencing employee behavior that is associated with employees’ feelings and reactions in the face of ethical issues [20]. The organization’s ethical climate reflects moral values, behavioral expectations, and the impact of ethics on members’ decisions, which provides a framework for ethical decision-making in clinical settings [21]. In other words, the ethical climate can act as a resource for employees that shapes their ethical attitudes and behaviors in the face of ethical challenges [20, 21]. It may also positively affect patient satisfaction, nursing practices, and ethical decision-making [22]. Hart’s descriptive study showed the relationship between a negative ethical climate and nurses’ decision to leave the nursing profession [23]. To date, findings suggest that an ethical climate may contribute to moral distress [19, 24], organizational commitment [25], turnover intentions, reduced job satisfaction [26], and unsafe patient care [17].
Although most studies on moral distress have been done with clinical nurses [17], it is not limited to nursing. Due to the unpredictable missions, time constraints, and locations involved, prehospital ambulance-based research has unique ethical issues than other emergency research departments [27]. According to the evidence, moral distress is influenced by personal characteristics, clinical situations, and organizational conditions [28], and ethical climate is also influenced by various factors, such as cultural, legal, and organizational regulations [29]. Also, the intensity and frequency of perceived moral distress experienced by EMS personnel and their ethical climate are affected by factors not comparable to in-hospital situations. Although several studies have been conducted on moral distress and healthcare professionals’ ethical climate [29, 30], none have been conducted on the level of moral distress and perception of ethical climate among prehospital EMS personnel in Iran. Accordingly, this study investigates the relationship between moral distress and the perceived ethical climate among EMS personnel.
The results of this study can play an essential role in better identifying factors affecting EMS employees’ moral distress. In addition, by identifying the ethical climate perceived by EMS staff, it is possible to apply the organization’s policies to improve job satisfaction and motivation, increase EMS service quality, and reduce moral distress. This study determined the relationship between ethical climate and moral distress among EMS personnel.
Materials and Methods
Study design and participants
This descriptive-correlational study was performed on EMS staff working in emergency medical centers affiliated with Hamadan University of Medical Sciences in Iran. The participants were selected via the census sampling method. A total of 136 EMS staff working in urban and road stations entered the study and completed the questionnaires. The inclusion criteria in this study included having at least a bachelor of science in nursing and medical emergency, and at least one year of working experience in EMS centers. Meanwhile, the exclusion criteria were having no history of high stress (death of relatives, family problems, and coronavirus infection in oneself or your family) in the past eight weeks.
Data collection
Before data collection, legal permits and coordination with the Medical Emergency and Accident Center authorities were obtained. Due to the wide dispersion of urban and road emergency bases and COVID-19 health protocols, the data were collected by an electronic survey. Data collection lasted from April to July 2020. The participants who had not responded within two weeks were sent an electronic reminder at weeks 2 and 6.
Study instruments
The study instrument consists of three parts as follows.
Demographic data
The demographic data included age, gender, marital status, clinical work experience, educational status, and employment status.
Moral distress instruments
Various tools are available to measure moral distress. The most common include the moral distress scale (MDS) [31], the moral distress scale-revised (MDS-R) [15], and the moral distress thermometer [32].
One of the predominant data-gathering methods in moral distress is the questionnaire, with Corley MDS [31, 33], based on Jameton’s theoretical definition. The Corley MDS is a 38-item scale that measures moral distress intensity (MDI) and moral distress frequency (MDF), ranging from 0 to 6 for each category.
The MDS-R consists of 21 items. It measures people’s perceptions of a situation based on the intensity of moral distress and the frequency of encountering it. In Iran, a psychometric evaluation of the MDS-R instrument was performed, and its reliability was confirmed using the Cronbach α [34].
The moral distress thermometer, with its 11-point scale (0-10), may be used as a screening tool for moral distress, which has less convergent validity than the moral distress instrument [32].
MDS-R is based on pre-hospital context. In this study, due to the different clinical contexts of EMS staff, some items of the MDS-R questionnaire were revised by reviewing specialized texts and qualitative studies in the field of EMS, as well as the opinions of experts in the field of EMS. Items unrelated to EMS (under pressure related to organizational costs and organ donation) were removed. Several items related to the EMS staff’s ethical distress (following orders, irrational requests from family members, caring in insecure situations, and legal conflicts) were replaced. Finally, MDS-R items for EMS reached a total of 24. MDI was scored using a 6-point Likert scale ranging from “not at all” (score 0) to “repeatedly” (score 5) and MDF with a range of “I have never experienced distress” (score 0) to “I experienced distress repeatedly” (score 5). This tool’s content validity was obtained after reviewing ten faculty members and five experts in EMS. The instrument’s reliability was measured using the Cronbach α of 0.94 and 0.91 for intensity and frequency, respectively.
Ethical climate instruments
Over time, several tools have been developed to examine ethical climate. The most common in medicine are the hospital ethical climate questionnaire (HECS) and the ethical climate questionnaire (ECQ).
Olson (1998) developed the HECS to assess nurses’ perception of the hospital’s ethical climate. The HECS consists of a 26-item survey with five subcategories (relationships with peers, patients, managers, hospital administrators, and physicians) scored on a 5-point Likert scale from 1 to 5 (1=almost never true to 5=almost always true) [35].
The ECQ was developed by Victor and Cullen (1988) and consisted of a 26-item tool that measures five types of ethical climate in an organization. In addition to instrumental, caring, independence, rules, and low and code climates, there are five ethical climates. The scoring of this questionnaire is based on the 6-point Likert scale ranging from 0=strongly disagree to 6=strongly agree [36].
A 12-item revised ethical climate questionnaire was developed for this study. According to Cullen et al. (1993), the moral distress frequency focuses on three factors of ethical criteria, namely egoism (maximizing one’s self-interests), benevolence (maximizing joint interests), and principled (adherence to universal principles) [37] to measure the agreement with each statement. The scale ranged from [1] strongly disagree to [5] strongly agree.
To examine the tool’s content validity, questionnaires were provided to experts in medical ethics. They were asked to check whether the tool statements were clear and adequately linked to the categorized dimensions. In addition, internal consistency reliability was 0.89 using the Cronbach α.
Results
Demographic characteristics
In this study, out of 154 eligible participants, 136 (88.3%) answered the questionnaire. Most of the participants were married (62%), had a bachelor’s degree in emergency medicine (58%), and had annual contract employment (47.8%). The average work experience of personnel was 10.2±3.4 years, ranging from 1 to 23 years. Their mean age was 33.4±3.54 years, ranging from 23 to 49 years. In addition, 24.2% of the personnel had a history of public complaints against them or were referred to the Board of Inquiry at least once (Table 1).
Moral distress and ethical climate
The mean MDI was 3.65±1.14 with a range of 4.83±0.62, and the mean MDF was 1.83±0.53 with a range of 3.49±0.25, which shows that the mean MDI and MDF are high and moderate, respectively. The most moral distress experienced by EMS staff was related to providing low-quality services due to high workload, having to comply with patients’ irrational requests, and caring in unsafe conditions. The mean ethical climate was moderate (2.96±1.02), with a range of 4.11±1.06. The highest score of ethical climates from the EMS staff’s perspective was related to adherence to principles, independence egoism, and benevolence, respectively. Among the questions, the highest score of ethical climates was related to the observance of professional rules and standards and the lowest score was related to the evaluation of individuals based on the organization’s interests and respecting others’ rights.
Relationship between demographic characteristics and moral distress
The results showed a significant relationship between the MDI and some personal characteristics, such as age, work experience, and having a history of referral to the Board of Inquiry (P<0.05). Accordingly, the most moral distress among employees under the age of 7 years (3.17±0.87), ages less than 28 years (3.23±1.03), and with a history of referral to the Board of Inquiry (2.14±0.57) was experienced (P<0.05). Also, moral distress in bachelor’s degree in emergency medicine (2.74±0.95) was more than in other disciplines. According to the findings, there was only a significant relationship between MDF and work experience (employees with less than seven years of experience) (P<0.05) (Table 1).
Relationship between demographic characteristics and ethical climate
The results indicated that demographic factors were not significantly related to ethical climate (P>0.05); however, the ethical climate among employees with a history of complaining or referring to the Board of Inquiry was lower than among other employees.
Relationship between moral distress intensity and moral distress frequency, and their relationship with ethical climate aspects
The results showed a negative and significant relationship between EC and EMS staff MDI (r=-0.34, P<0.05). However, there was no significant relationship between EC and MDF (r=-0.11, P>0.05). Based on the results, MDI was only related to the dimension of adherence to universal principles (principled). Nevertheless, MDF had no significant relationship with any of the dimensions of ethical climate (Table 2).
Multiple analyses of the relationship between variables simultaneously with moral distress
The relationship between ethical climate with the MDI and MDF using multiple linear regression analysis showed that 32.8% of the MDI is explained by ethical climate (F=13.53, R2=0.328, P<0.001) and 4.7% of the MDF is explained by ethical climate (F=1.21, R2=0.047, P>0.05) (Table 3).
At the end of the moral distress questionnaire, EMS personnel were asked to describe the most common cause of their moral distress. Some of them described moral distress in an emergency. One of them described the situation in which the injured person asked us to tell the health status of other family members in the car accident. However, it was difficult to announce family members’ deaths. Another staff member described his experiences as often asking us to perform treatment at home and not to transport their patient to the hospital due to poor financial circumstances. Some employees have pointed out that announcing bad news or family death is a common issue that causes severe distress. Other EMS staff cited challenges such as scene insecurity, inappropriate family requests, and threats to sue.
Discussion
The findings showed a significant negative relationship between MDI and the ethical climate among EMS personnel. Therefore, a positive ethical climate can reduce MDI among EMS personnel. In this regard, Lützén et al. (2010) found that ethical climate predicts and explains 33.7% of moral distress through linear regression analyses with some moral sensitivity items [18]. Some studies found a significant negative correlation between moral distress and ethical climate, indicating that a poor ethical climate is associated with higher moral distress [17, 30, 33]. Additionally, Schluter (2008) found that moral distress is inevitable in an ethical climate where the priorities are perceived to be budget and patient throughput over patient safety [21]. Janvier et al. reported that the level of moral distress among nurses depends on the work environment [38]. Additionally, Schluter et al. found that moral distress is inevitable in an ethical climate where the priorities are perceived to be budget and patient throughput over patient safety [21]. According to an ethical analysis in 2022, moral distress can undermine a physician’s ethical integrity, leading to anger, poor job satisfaction, reduced quality of care, and burnout. The analysis suggested that addressing an ethical climate could help reduce moral distress among healthcare professionals [39]. Asgari et al. and Hou et al. found that a positive ethical climate predicted lower moral distress in critical care nurses and emergency department nurses, respectively [30, 40]. Similarly, Pauly (2009) found that each aspect of ethical climate (peers, patients, managers, hospitals, and physicians) was significantly correlated with moral distress in a random sample of registered nurses [17]. However, Altaker et al. (2018) found no relationship between moral distress and ethical climate in intensive care unit nurses [41].
The results of Asgari et al. (2017), also using regression analysis, showed that among the studied variables (age, sex, work experience, marriage, job position, and ethical climate), there is only a significant relationship between ethical climate and moral distress [30]. Also, similar to our findings, several studies indicate that nurses who perceived a more positive ethical climate experienced less moral distress; therefore, EMS staff on two-person out-of-hospital missions have to make quick ethical decisions in unsafe and unpredictable situations, leading to more moral distress than in-hospital nurses. However, despite the special pre-hospital emergency conditions and the ethical climate different from hospitals, a positive ethical climate can significantly reduce EMS staff’s moral distress.
According to our study, EMS staff experienced a high level of MDI. This was often related to increased workload, unreasonable patient requests, and providing care services under unsafe conditions. Also, the mean MDF was reported to be moderate, often associated with a high workload, limited career advancement opportunities, and following superior orders. Ruston et al. (2015) indicated that employees should identify barriers to moral distress in themselves and their organization. For EMS providers, this can include the instability of the work environment, how decisions are made, interpersonal interactions, and maintaining the respect and dignity of employees within the organization [42]. Vazir et al. found that the severity of moral distress in the EMS, intensive care units, and neonatal intensive care unit staff is higher than in the other departments of internal medicine, ophthalmology, and ear, nose, and throat [43]. Jafari et al. showed that about 76% of the technicians working in EMS experienced a moderate level of moral distress [44]. In line with the present study, Salari et al. reported in a systematic review and meta-analysis that the intensity and frequency of moral distress in nurses is high [45].
Studies have also demonstrated that moral distress is prevalent among EMS staff, including emergency department nurses, due to the challenging nature of their work [46, 47]. The level of moral distress EMS staff experience depends on their role and workplace environment. ED nurses tend to experience higher moral distress than physicians, likely because they are more directly involved in patient care [40]. Staff in intensive care units and emergency departments also experience greater moral distress than those in non-critical care settings, due to the high-stakes nature of the work [40, 48].
The results of studies have shown that various factors, such as following the patients’ or families’ irrational requests, conflict of values, conflict of ethics and law, and the lack of experience are among the ethical EMS personnel challenges in their ethical decision-making [3, 4], which is consistent with some of the items of moral distress in the present study. Also, a study demonstrated that EMS personnel’s moral distress was more related to feelings of disrespect, performance in a hostile moral environment, and acting against the patient’s best interests [49]. The MDF was lower than its intensity in the present study, consistent with some studies [17, 19]. The results of the present study showed that the mean EMS personnel’s ethical climate is moderate, which is often related to adherence to principles. The results of Jalali et al. (2017) also showed that the mean ethical climate among EMS staff is at a desirable level, often related to professionalism and adherence to rules [50], consistent with the present study. According to the findings, EMS staff, like hospital nurses, seem more ethically motivated by regulations.
This study showed a significant relationship between increasing age, experience, and no complaints history or referral to the Board of Inquiry for violations, reducing moral distress intensity. In this regard, the results of some studies indicate no significant relationship between demographic characteristics and moral distress [51, 52]. Silén et al. also showed that nurses with less than six years of work experience have less moral distress than nurses with more work experience [19], which is not consistent with the findings of the present study.
The inverse relationship between work experience and history of reporting EMS staff misconduct with moral distress may be related to the impact of training classes and staff familiarity with ethical principles, standards, and rules. The experiences of EMS staff in ethical decision-making have also shown that fear of complaint, the lack of manager support, and low expertise are among the ethical decision-making barriers and create moral distress [4].
Also, according to the findings, no demographic characteristics have a significant relationship with the EMS staff’s ethical climate, consistent with some studies [17, 53].
Due to the occupational nature of medical emergencies and the cultural and organizational characteristics of prehospital emergency medical centers in Iran, it is difficult to accurately examine the relationship between the variables of ethical climate and moral distress perceived by EMS staff. Since little research has been done on ethical issues in EMS in Iran, more quantitative and qualitative research is needed to explore the factors related to moral distress and ethical climate among EMS personnel.
The findings can provide valuable information to prehospital supervisors and managers in identifying the contributing factors to moral distress from the perspective of EMS staff. The findings may also help managers plan to improve the organization’s ethical climate and ultimately increase prehospital care quality by reducing moral distress.
Conclusion
This study investigated perceived moral distress and ethical climate among EMS personnel and the associations between the MDI and MDF and different aspects of ethical climate. Accordingly, EMS personnel perceived a moderate ethical climate. The highest scores for ethical climate included adherence to principles, egoism, and benevolence, respectively. The findings showed that the mean MDI was high, while the mean MDF was moderate. The most common cause of moral distress was related to providing low-quality services due to high workload, having to comply with patients’ irrational requests, and caring in unsafe conditions. The study found a significant relationship between MDI and some personal characteristics, such as age, work experience, and having a history of referral to the Board of Inquiry. However, there was only a significant relationship between work experience and MDF. On the other hand, demographic factors did not have a significant relationship with ethical climate, except for employees with a history of complaining or referring to the research board, who had a lower ethical climate. The findings showed that a positive ethical climate could reduce EMS staff’s MDI. Therefore, to reduce moral distress and improve the ethical climate among EMS personnel, the following is recommended: Attention to the organization’s interests in evaluating employees, revision and review of employee complaints in referral to the Board of Inquiry, reduction of workload by increasing the number of emergency bases, and adjusting expectations of employees according to their circumstances.
Study limitations
Even though enough studies have been conducted to investigate the moral distress and ethical climate of nurses working in hospitals, the results reported in this study may not be generalizable to EMS personnel. Also, despite validating these questionnaires on prehospital workers, more comprehensive research with different cultural and ethnic characteristics in different countries is necessary to confirm the generalizability of the findings.
Ethical Considerations
Compliance with ethical guidelines
Ethical approval was received from the Ethics Committee of Hamadan University of Medical Sciences (Code: IR.UMSHA.REC.1398.578). Informed consent was obtained from all participants to participate in the study, and they were assured that the information would remain confidential.
Funding
This study was conducted with the support of the Vice Chancellor for Research and Technology at Hamadan University of Medical Sciences (Project No.: 9807305714).
Authors' contributions
All authors equally contributed to preparing this article.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors would like to express their gratitude to all the emergency medical staff at the Accident and Emergency Medical Center who assisted us in this study.
References
- Zavotsky KE, Chan GK. Exploring the relationship among moral distress, coping, and the practice environment in emergency department nurses. Advanced Emergency Nursing Journal. 2016; 38(2):133-46. [DOI:10.1097/TME.0000000000000100]
- Blanchard IE, Doig CJ, Hagel BE, Anton AR, Zygun DA, Kortbeek JB, et al. Emergency medical services response time and mortality in an urban setting. Prehospital Emergency Care. 2012; 16(1):142-51. [DOI:10.3109/10903127.2011.614046]
- Torabi M, Borhani F, Abbaszadeh A, Atashzadeh-Shoorideh F. Experiences of pre-hospital emergency medical personnel in ethical decision-making: A qualitative study. BMC Medical Ethics. 2018; 19(1):95. [DOI:10.1186/s12910-018-0334-x] [PMID]
- Torabi M, Borhani F, Abbaszadeh A, Atashzadeh-Shoorideh F. Barriers to ethical decision-making for pre-hospital care professionals. Nursing Ethics. 2020; 27(2):407-18. [DOI:10.1177/0969733019848044]
- Roden-Foreman JW, Bennett MM, Rainey EE, Garrett JS, Powers MB, Warren AM. Secondary traumatic stress in emergency medicine clinicians. Cognitive Behaviour Therapy. 2017; 46(6):522-32. [DOI:10.1080/16506073.2017.1315612]
- Torabi M, Borhani F, Abbaszadeh A, Atashzadeh-Shoorideh F. Ethical decision-making based on field assessment: The experiences of prehospital personnel. Nursing Ethics. 2019; 26(4):1075-86. [DOI:10.1177/0969733017736925]
- Mahdavi Fashtami S, Mohammadeh Zadeh Zarankesh S, Esmaeilpour Bandboni M. [Moral distress among emergency department nurses: Frequency, intensity, effect (Persian)]. Medical sciences. 2016; 26(4):248-55. [Link]
- Jameton A. Nursing practice: The ethical issues. Hoboken Hoboken: Prentice Hall; 1984. [Link]
- American Association of Critical Care Nurses (AACN). AACN position statement moral distress in times of crisis. Aliso Viejo: AACN; 2008. [Link]
- Varcoe C, Doane G, Pauly B, Rodney P, Storch JL, Mahoney K, et al. Ethical practice in nursing: Working the in-betweens. Journal of Advanced Nursing. 2004; 45(3):316-25. [DOI:10.1046/j.1365-2648.2003.02892.x]
- Becker TK, Gausche-Hill M, Aswegan AL, Baker EF, Bookman KJ, Bradley RN, et al. Ethical challenges in emergency medical services: Controversies and recommendations. Prehospital and Disaster Medicine. 2013; 28(5):488-97. [DOI:10.1017/S1049023X13008728]
- Pavlish C, Brown-Saltzman K, Hersh M, Shirk M, Rounkle AM. Nursing priorities, actions, and regrets for ethical situations in clinical practice. Journal of Nursing Scholarship. 2011; 43(4):385-95. [DOI:10.1111/j.1547-5069.2011.01422.x]
- Rushton CH, Caldwell M, Kurtz M. CE: Moral distress: A catalyst in building moral resilience. AJN: American Journal of Nursing. 2016; 116(7):40-9. [DOI:10.1097/01.NAJ.0000484933.40476.5b]
- Brazil K, Kassalainen Sh, Ploeg J, Marshall D. Moral distress experienced by health care professionals who provide home-based palliative care. Social Science & Medicine. 2010; 71(9):1687-91. [DOI:10.1016/j.socscimed.2010.07.032]
- Hamric AB, Borchers CT, Epstein EG. Development and testing of an instrument to measure moral distress in healthcare professionals. AJOB Primary Research. 2012; 3(2):1-9. [DOI:10.1080/21507716.2011.652337]
- Zuzelo PR. Exploring the moral distress of registered nurses. Nursing Ethics. 2007; 14(3):344-59. [DOI:10.1177/0969733007075870]
- Pauly B, Varcoe C, Storch J, Newton L. Registered nurses’ perceptions of moral distress and ethical climate. Nursing Ethics. 2009; 16:561-73. [DOI:10.1177/0969733009106649]
- Lützén K, Blom T, Ewalds-Kvist B, Winch S. Moral stress, moral climate and moral sensitivity among psychiatric professionals. Nursing Ethics. 2010; 17(2):213-24. [DOI:10.1177/0969733009351951]
- Silén M, Svantesson M, Kjellström S, Sidenvall B, Christensson L. Moral distress and ethical climate in a Swedish nursing context: Perceptions and instrument usability. J Clin Nurs. 2011; 20(23-24):3483-93. [DOI:10.1111/j.1365-2702.2011.03753.x]
- Atabay G, Çangarli BG, Penbek Ş. Impact of ethical climate on moral distress revisited: Multidimensional view. Nursing Ethics. 2015; 22(1):103-16. [DOI:10.1177/0969733014542674]
- Schluter J, Winch S, Holzhauser K, Henderson A. nurses’ moral sensitivity and hospital ethical climate: A literature review. Nursing Ethics. 2008; 15(3):304-21. [DOI:10.1177/0969733007088357]
- Cerit B, Özveren H. Effect of hospital ethical climate on the nurses’ moral sensitivity. The European Research Journal. 2019; 5(2):282-90. [DOI:10.18621/eurj.423324]
- Hart SE. Hospital ethical climates and registered nurses’ turnover intentions. Journal of Nursing Scholarship. 2005; 37:173-7. [DOI:10.1111/j.1547-5069.2005.00030.x]
- Sauerland J, Marotta K, Peinemann MA, Berndt A, Robichaux C. Assessing and addressing moral distress and ethical climate, part 1. Dimensions of Critical Care Nursing. 2014; 33(4):234-45. [DOI:10.1097/DCC.0000000000000050]
- Ismail S. Effects of ethical climate on organizational commitment, professional commitment, and job satisfaction of auditor in Malaysia. Gadjah Mada International Journal of Business. 2015; 17:139-55. [DOI:10.22146/gamaijb.6907]
- Abou Hashish EA. Relationship between ethical work climate and nurses’ perception of organizational support, commitment, job satisfaction and turnover intent. Nursing Ethics. 2017; 24(2):151-66. [DOI:10.1177/0969733015594667]
- Sporrong SK, Höglund AT, Arnetz B. Measuring moral distress in pharmacy and clinical practice. Nursing Ethics. 2006; 13(4):416-27. [DOI:10.1191/0969733006ne880oa]
- Hamric AB, Blackhall LJ. Nurse-physician perspectives on the care of dying patients in intensive care units: Collaboration, moral distress, and ethical climate. Critical Care Medicine. 2007; 35(2):422-9. [DOI:10.1097/01.CCM.0000254722.50608.2D]
- Huang CC, You CS, Tsai MT. A multidimensional analysis of ethical climate, job satisfaction, organizational commitment, and organizational citizenship behaviors. Nursing Ethics. 2012; 19(4):513-29. [DOI:10.1177/0969733011433923]
- Asgari S, Shafipour V, Taraghi Z, Yazdani-Charati J. Relationship between moral distress and ethical climate with job satisfaction in nurses. Nursing Ethics. 2019; 26(2):346-56.[DOI:10.1177/0969733017712083]
- Corley MC, Elswick RK, Gorman M, Clor T. Development and evaluation of a moral distress scale. Journal of Advanced Nursing. 2001; 33(2):250-6. [DOI:10.1046/j.1365-2648.2001.01658.x]
- Wocial LD, Weaver MT. Development and psychometric testing of a new tool for detecting moral distress: The Moral Distress Thermometer. Journal of Advanced Nursing. 2013; 69(1):167-74. [DOI:10.1111/j.1365-2648.2012.06036.x]
- Corley MC, Minick P, Elswick RK, Jacobs M. Nurse moral distress and ethical work environment. Nursing Ethics. 2005; 12(4):381-90. [DOI:10.1191/0969733005ne809oa]
- Soleimani MA, Sharif SP, Yaghoobzadeh A, Panarello B. Psychometric evaluation of the Moral Distress Scale–Revised among Iranian nurses. Nursing Ethics. 2019; 26(4):1226-42. [DOI:10.1177/0969733016651129]
- Olson LL. Hospital nurses’ perceptions of the ethical climate of their work setting. Image: The Journal of Nursing Scholarship. 1998; 30(4):345-9. [DOI:10.1111/j.1547-5069.1998.tb01331.x]
- Victor B, Cullen JB. The organizational bases of ethical work climates. Administrative Science Quarterly. 1988; 33(1):101-25. [DOI:10.2307/2392857]
- Cullen JB, Victor B, Bronson JW. The ethical climate questionnaire: An assessment of its development and validity. Psychological Reports. 1993; 73(2):667-74. [DOI:10.2466/pr0.1993.73.2.667]
- Janvier A, Nadeau S, Deschênes M, Couture E, Barrington KJ. Moral distress in the neonatal intensive care unit: Caregiver’s experience. Journal of Perinatology. 2007; 27:203-8. [DOI:10.1038/sj.jp.7211658]
- Kherbache A, Mertens E, Denier Y. Moral distress in medicine: An ethical analysis. Journal of Health Psychology. 2022; 27(8):1971-90. [DOI:10.1177/13591053211014586]
- Hou Y, Timmins F, Zhou Q, Wang J. A cross-sectional exploration of emergency department nurses’ moral distress, ethical climate and nursing practice environment. International Emergency Nursing. 2021; 55:100972. [DOI:10.1016/j.ienj.2021.100972]
- Altaker KW, Howie-Esquivel J, Cataldo JK. Relationships among palliative care, ethical climate, empowerment, and moral distress in intensive care unit nurses. American Journal of Critical Care. 2018; 27(4):295-302. [DOI:10.4037/ajcc2018252]
- Rushton CH, Batcheller J, Schroeder K, Donohue P. Burnout and resilience among nurses practicing in high-intensity settings. American Journal Critical Care. 2015; 24(5):412–20. [DOI:10.4037/ajcc2015291]
- Vaziri MH, Merghati-Khoei E, Tabatabaei S. Moral distress among Iranian nurses. Iranian Journal of Psychiatry. 2015; 10(1):32-6. [PMID]
- Jafari M, Khankeh H, Ebadi A, Maddah SSB, Hosseini M. Moral distress in pre-hospital emergency technicians: A cross-sectional study in Iran. Health in Emergencies and Disasters Quarterly. 2023; 8(4):323-8. [DOI:10.32598/hdq.8.4.467.1]
- Salari N, Shohaimi S, Khaledi-Paveh B, Kazeminia M, Bazrafshan MR, Mohammadi M. The severity of moral distress in nurses: A systematic review and meta-analysis. Philosophy, Ethics, and Humanities in Medicine. 2022; 17:13. [DOI:10.1186/s13010-022-00126-0]
- Jafari M, Hosseini MA, Bagher Maddah S, Khankeh HR, Ebadi A. Factors behind moral distress among Iranian emergency medical services staff: A qualitative study into their experiences. Nursing and Midwifery Studies. 2019; 8:195-202. [Link]
- Fernandez-Parsons R, Rodriguez L, Goyal D. Moral distress in emergency nurses. Journal of Emergency Nursing. 2013; 39(6):547-52. [DOI:10.1016/j.jen.2012.12.009]
- Donkers MA, Gilissen VJHS, Candel MJJM, van Dijk N, Kling H, Heijnen-Panis R, et al. Moral distress and ethical climate in intensive care medicine during COVID-19: A nationwide study. BMC Medical Ethics. 2021; 22:73. [DOI:10.1186/s12910-021-00641-3]
- Viele CM. Moral distress in emergency medical services [MSc thesis]. Maryland: Johns Hopkins University; 2018. [Link]
- Jalali T, Borhani F, Esmailpur H, Aliesmaeli M, Aminizade M, Motamed Jahromi M. [Relationship between ethical climate and organizational commitment of medical emergency technicians in Kerman University of Medical Sciences (Persian)]. Iranian Journal of Medical Ethics and History of Medicine. 2017; 10:91-102. [Link]
- Allari R, Abu-Moghli F. Moral distress among Jordanian critical care nurse and their perception of hospital ethical climate. Journal of Natural Sciences Research. 2013; 3(5):144-54. [Link]
- O’Connell CB. Gender and the experience of moral distress in critical care nurses. Nursing Ethics. 2015; 22(1):32-42.[DOI:10.1177/0969733013513216]
- Parker FM, Lazenby RB, Brown JL. The relationship of moral distress, ethical environment and nurse job satisfaction. Journal of Health Ethics. 2013; 10(1). [DOI:10.18785/ojhe.1001.02]
Type of article: Research |
Subject:
Special
Received: 2023/09/13 | Accepted: 2023/12/18 | Published: 2024/04/1
Received: 2023/09/13 | Accepted: 2023/12/18 | Published: 2024/04/1
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |





