Volume 9, Issue 3 (Spring 2024)
Health in Emergencies and Disasters Quarterly 2024, 9(3): 159-172 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Seyghalani Talab F, Ahadinezhad B, Khosravizadeh O. Investigating the Organizational Resilience of Hospitals During Emergencies and Disasters: A Comprehensive Review of the Components. Health in Emergencies and Disasters Quarterly 2024; 9 (3) :159-172
URL: http://hdq.uswr.ac.ir/article-1-570-en.html
URL: http://hdq.uswr.ac.ir/article-1-570-en.html
1- Student Research Committee, Qazvin University of Medical Sciences, Qazvin, Iran., 1. Student Research Committee, Qazvin University of Medical Sciences, Qazvin, Iran
2- Social Determinants of Health Research Center, Research Institute for Prevention of Non-Communicable Diseases, Qazvin University of Medical Sciences, Qazvin, Iran., 2. Social Determinants of Health Research Center, Research Institute for Prevention of Non-Communicable Diseases, Qazvin University of Medical Sciences, Qazvin, Iran
3- Social Determinants of Health Research Center, Research Institute for Prevention of Non-Communicable Diseases, Qazvin University of Medical Sciences, Qazvin, Iran. ,omid.khosravizadeh@gmail.com
2- Social Determinants of Health Research Center, Research Institute for Prevention of Non-Communicable Diseases, Qazvin University of Medical Sciences, Qazvin, Iran., 2. Social Determinants of Health Research Center, Research Institute for Prevention of Non-Communicable Diseases, Qazvin University of Medical Sciences, Qazvin, Iran
3- Social Determinants of Health Research Center, Research Institute for Prevention of Non-Communicable Diseases, Qazvin University of Medical Sciences, Qazvin, Iran. ,
Full-Text [PDF 679 kb]
(1137 Downloads)
| Abstract (HTML) (3481 Views)
Full-Text: (1004 Views)
Introduction
Disasters can disturb a wide array of infrastructures and facilities, ranging from hospitals to educational institutions, transportation networks, and emergency services. Meanwhile, hospitals play a crucial role in critical circumstances as they mitigate the impact of such situations and decrease fatalities resulting from them [1]. As a result, efficient disaster management within hospitals is considered an essential approach to ensuring uninterrupted healthcare services amid crises, even when hospitals are directly impacted by such situations [2]. To manage crises effectively, a systematic procedure is required for executing organizational choices, enacting policies, devising solutions, and harnessing societal capabilities. This process mitigates the impact and detrimental outcomes of disasters. Among the pivotal phases of health-related crisis management is the capacity of the healthcare and treatment system to foster resilience, ensuring the provision of health and treatment services [3]. Conversely, hospital resilience is characterized as the hospitals’ capability to withstand, assimilate, and react to the impacts of critical circumstances, while upholding the continuity of vital health services and subsequently restoring the original state or adjusting to novel conditions. This description alludes to a holistic outlook on the hospital’s capacity to address urgent scenarios, encompassing inherent robustness (the capacity to endure and assimilate crises) and adaptable versatility (approaches to sustain the provision of crucial health services and adjust to forthcoming crises) [4]. Hence, assessing and communicating the status of hospitals and clinics constitutes the initial stride in readying them for emergencies and disasters. This evaluation encompasses identifying hazards, assessing both structural and non-structural vulnerabilities, evaluating functional preparedness, and considering diverse human and logistical capabilities as the primary measures to enhance hospitals’ preparedness to face accidents and crises [5, 6]. Regularly performing this assessment can furnish the necessary information and steps to enhance the effectiveness of health and treatment systems. To achieve this goal, it is essential to have a clear understanding of existing capacities, enabling the formulation of plans and actions that leverage these capacities to enhance the system’s resilience [6, 7]. As indicated earlier, the necessity to secure the uninterrupted provision of services within organizations has attained its pinnacle significance, given that it is of utmost importance to ascertain the capacity of organizations to handle emergencies and disasters [6]. Possessing a proficient initiative in appraising resilience management holds a pivotal position in ensuring the triumph of the continuity of organizational operations. Past instances have demonstrated that entities lacking a consistent and systematic strategy for overseeing hazardous processes have encountered numerous emergencies and disasters, leading to human casualties, financial setbacks, and environmental detriment [3]. Given that disturbances and discrepancies within hospitals can result in irreparable harm and losses, it becomes highly crucial to motivate researchers and decision-makers to develop remedies aimed at enhancing resilience within health and treatment facilities [8]. Considering the significance of hospitals’ continuous provision of services and the value of assessment, monitoring, and planning to enhance hospitals’ resilience against accidents, along with a review of relevant studies, the present research investigates the constituents of organizational resilience within hospitals during times of emergency and disasters.
Materials and Methods
Study design
This investigation was carried out as a comprehensive review aimed at identifying the organizational resilience elements of hospitals during crisis and disaster occurrences in 2022.
Research question and framework
The current study addresses this question “What constitutes organizational resilience elements within hospitals during emergencies and disasters?” It is structured around a multi-part conceptual framework, as depicted in Figure 1.
Search strategy
The data was collected by consulting PubMed, Web of Science, Magiran, SID, and Irandoc databases from 2012 to 2022. To identify and cover more articles, a manual search of some key authoritative journals was also done. The keywords included “sustainability”, “resilience”, “strategy”, “medical centers”, “healthcare”, “hospital”, “organizational resilience”, “crisis”, “disaster”, “emergency”, “health services”, “medical services”, and “health system” (Table 1).

“AND”, “or”, and “not” operators were used to combine or limit the search results.
Inclusion and exclusion criteria
To select the articles pertinent to the research domain, the criteria for inclusion comprised the following items: 1) Studies carried out within the last decade in the realm of hospital organizational resilience; 2) All types of descriptive, analytical, and cross-sectional studies that utilize various methodologies; and 3) Studies written only in the English and Persian languages. Meanwhile, the exclusion criteria were studies that were done in other service areas and studies that were not accessible.
Screening and selection of studies
Articles featuring keywords within their titles and abstracts were picked, followed by the identification and elimination of duplicate articles from the review procedure. Subsequently, the abstracts were assessed, followed by a thorough examination of the complete texts of the articles. Studies that aligned poorly with the study objectives and incorporated exclusion criteria were recognized and excluded. Ultimately, a compilation of titles for all the articles sourced from the database was generated. To establish the most fitting inventory, a screening process was conducted, during which irrelevant articles were eliminated. Lastly, the chosen articles were incorporated into the study. The selected articles were meticulously examined and assessed. The categorization and arrangement of titles, along with the detection and elimination of duplicate entries, were all facilitated through resource management software (EndNote X6).
Quality assessment and data extraction
Following the search, the gathered articles underwent evaluation by the researchers utilizing the strengthening of the reporting of observational studies in the epidemiology checklist. Articles of high quality were chosen by this assessment. This checklist stands as one of the prime instruments employed to assess the quality of observational articles. This checklist comprises 22 criteria spanning sections such as title, introduction, methodology, results, discussion, and conclusion. Articles failing to meet over 50% of the checklist criteria were excluded. Data extraction was carried out after the quality assessment. Necessary data, including author and year of publication, study location, study title, target population, study type, methodology, and key findings were extracted and succinctly summarized.
Category of results
The elements extracted in this study were organized into distinct dimensions. During this analysis, the re searchers individually classified the extracted components from the studies into various dimensions. Subsequently, the formulated dimensions and components were juxtaposed, and the researchers harmonized and presented a unanimous categorization. Then, the established dimensions and components were juxtaposed, and the researchers collated and presented a mutually agreed-upon singular classification.
Results
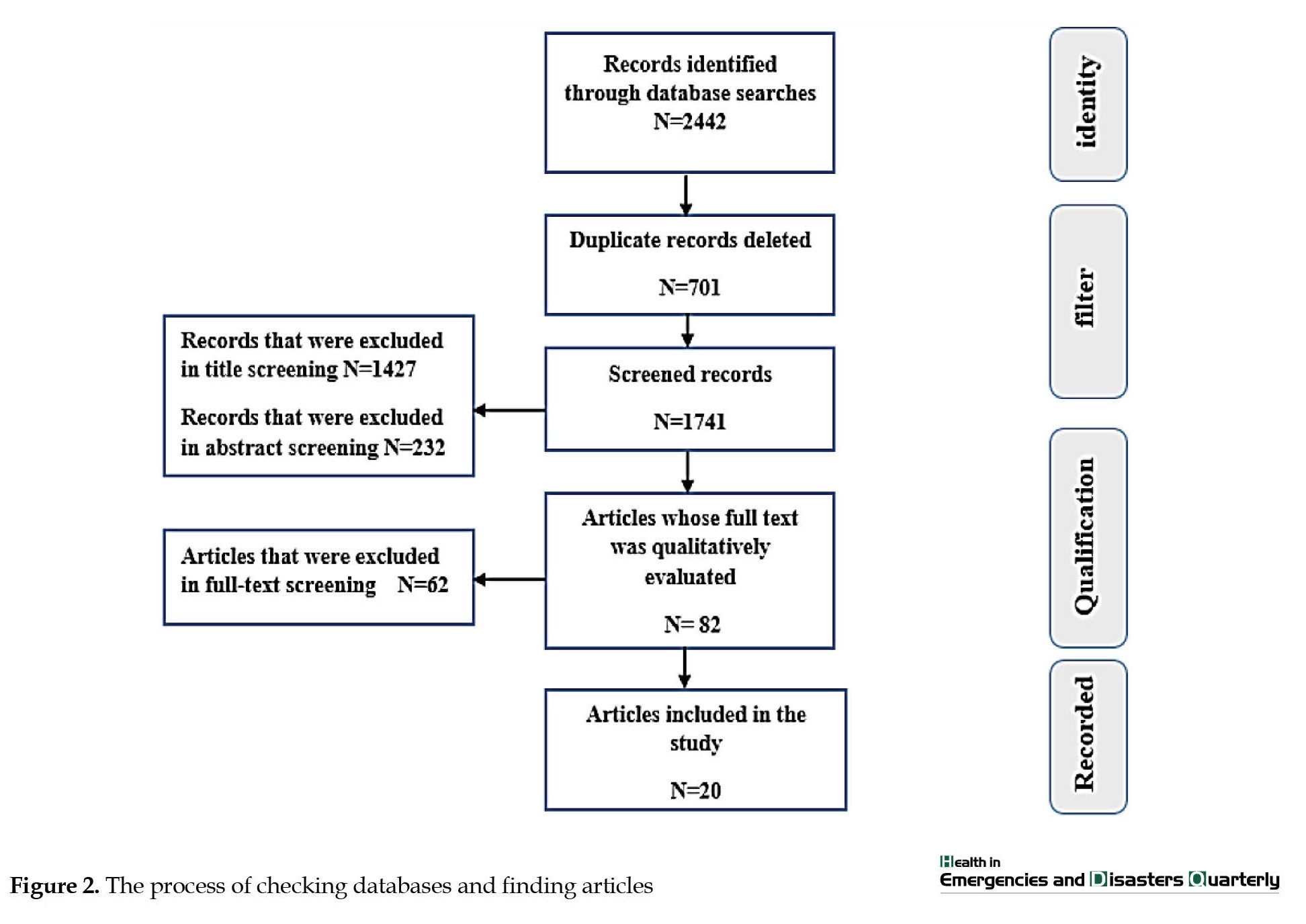
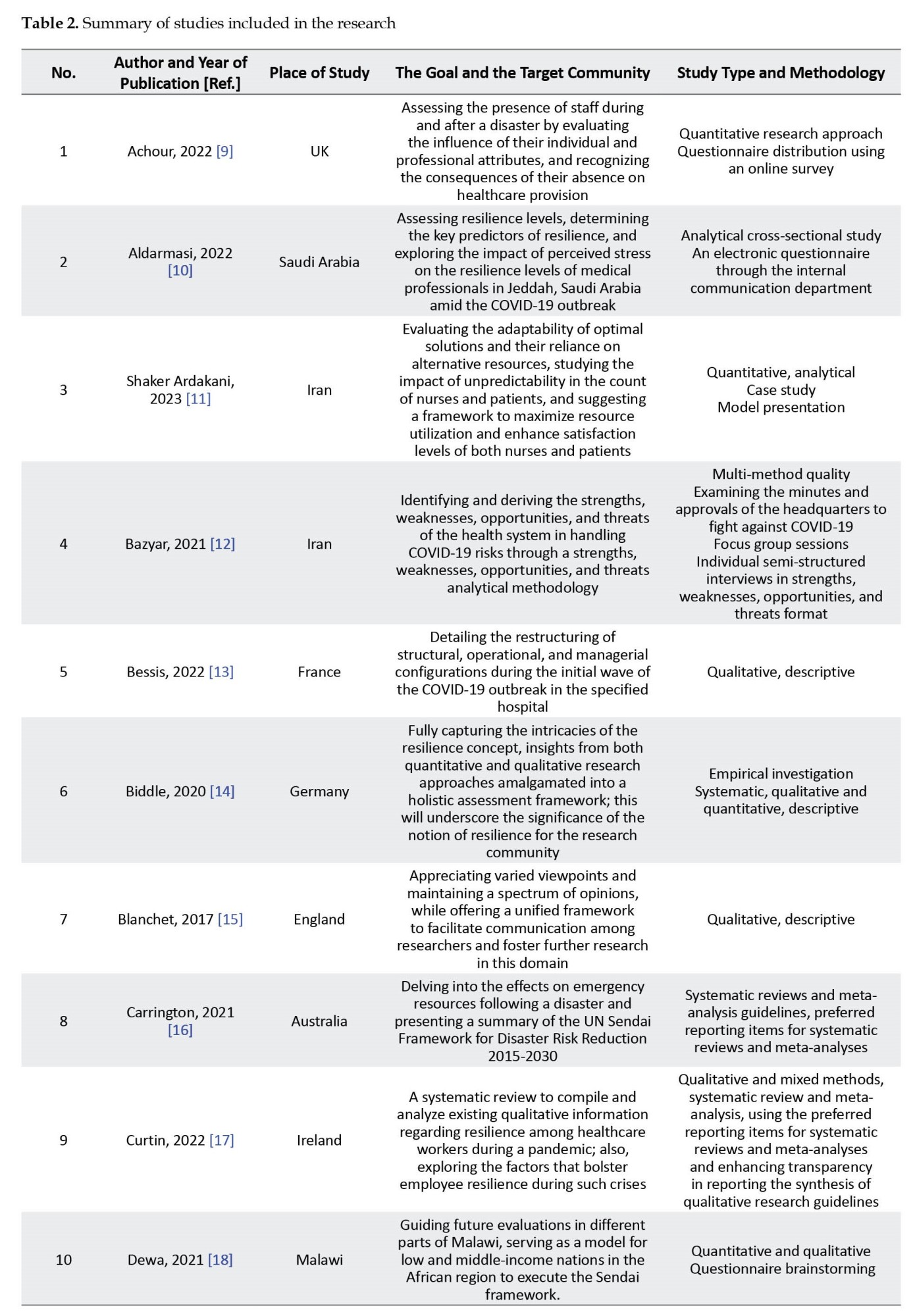
Several studies were conducted at different stages of the research, and 2442 studies were identified from the database search. An initial 701 articles were excluded due to their lack of titles pertinent to the study objectives, redundancy, and unavailability of the full article text. In the subsequent phase, after reviewing the abstracts of the articles, a total of 1659 articles were eliminated from consideration due to their lack of results relevant to our objectives. In the third stage, by studying the full text of the remaining articles, 62 articles were excluded due to the existence of similar Persian and English versions, being unrelated to the topic, and not having the necessary quality. Ultimately, a total of 20 articles that exhibited the closest alignment to the research topic were incorporated into the final analysis (Figure 2). The research examined a total of 20 final articles, consisting of 15 foreign studies and 5 domestic studies. Table 2 provides a summary of the reviewed studies, presenting various information, such as the article title, authors’ names, year of publication, study purpose and population, and the study type and methodology.

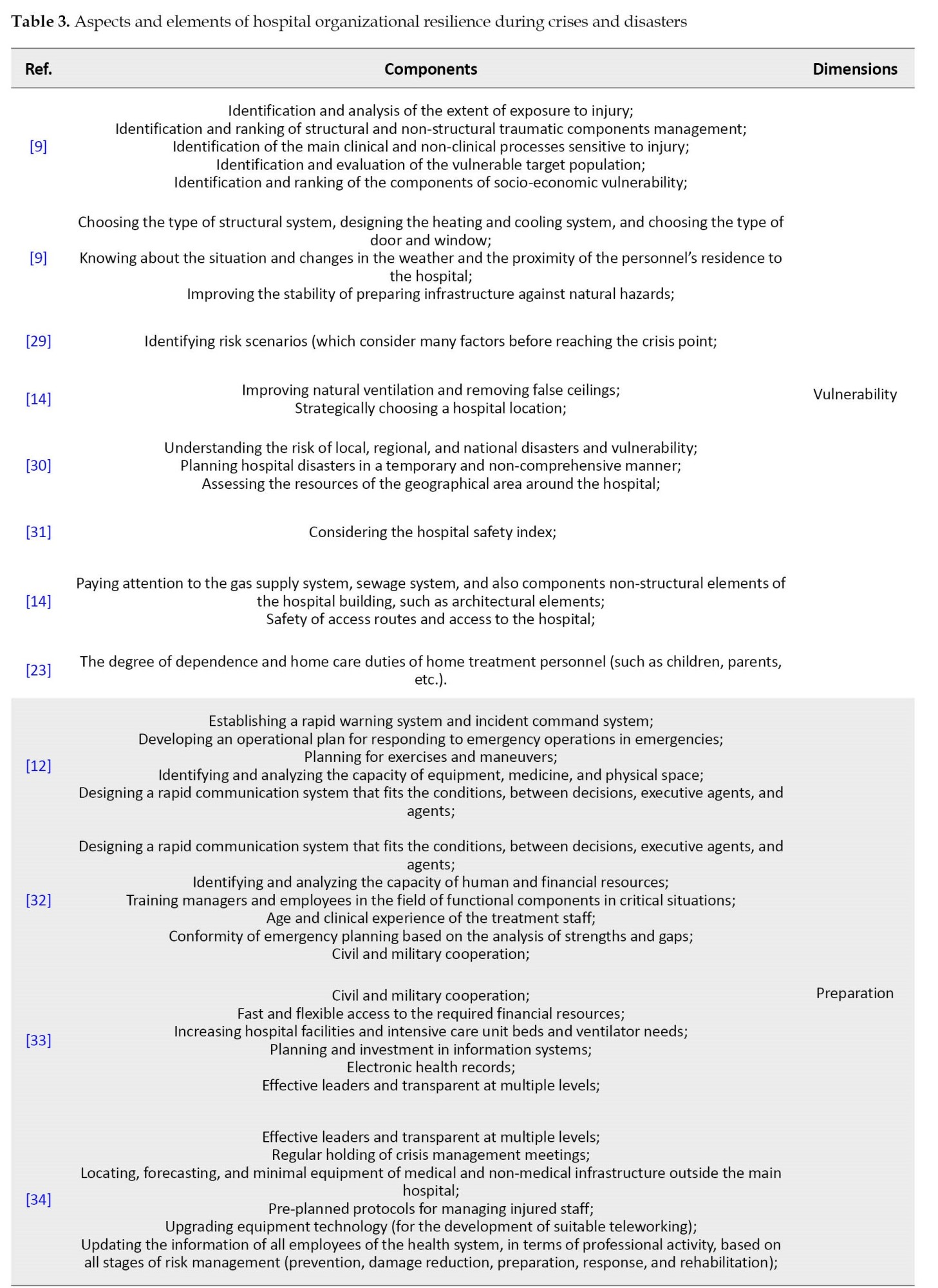
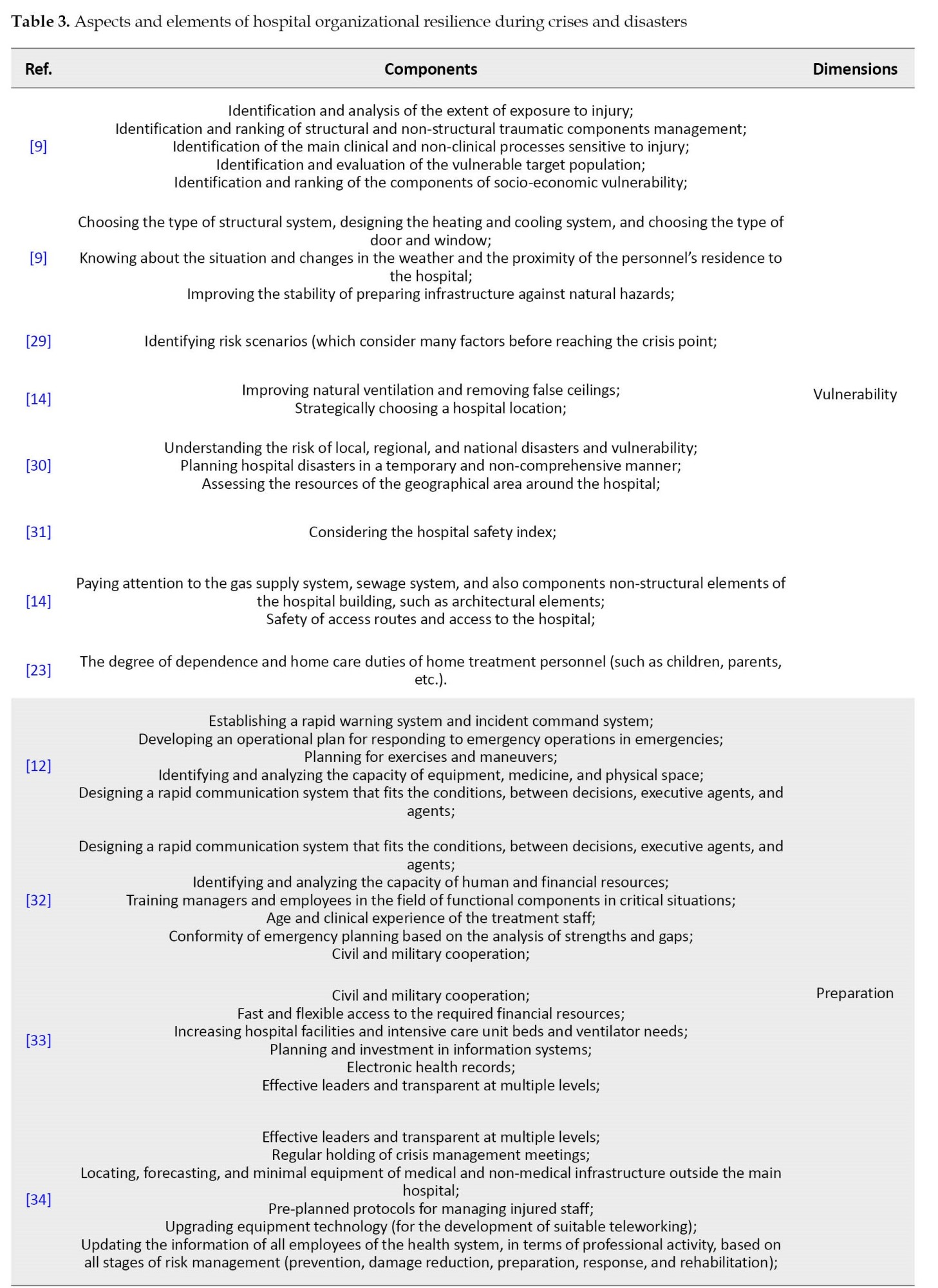
After closely analyzing 20 selected articles, the components of organizational resilience for hospitals during crises and disasters were categorized into five dimensions as follows: Vulnerability, preparedness, support management, responsiveness and adaptability during an emergency, and recovery after the emergency. The vulnerability dimension encompasses the recognized weaknesses that a set possesses about certain risks. A hospital’s vulnerability is influenced by its preparedness level. For instance, if a hospital is highly prepared for an earthquake, its susceptibility to it diminishes correspondingly. The preparedness dimension pertains to the idea of anticipating issues in human performance and indicates how the organization responds to significant incidents and crises, along with executing strategies in this area. It oversees the management of assistance, provision of resources, and other essential items needed to attain the operational objectives set by the incident command. Additionally, during a crisis, the response and adaptability phase is when the plan to address incidents is genuinely activated, to preserve human lives, offering first aid, mitigating and repairing system damages, and delivering necessary services to the victims. In essence, adaptability during a crisis means accelerating improvements. This is a crucial function of the hospital. Lastly, post-crisis recovery encompasses all actions undertaken to bring the hospital back to its pre-incident state. This procedure involves rebuilding existing buildings and infrastructures, restoring sub-structures, resettling the community, and offering essential mental health services to those who survived. The elements identified in the articles have been categorized and presented according to pre-established dimensions (Table 3).


Discussion
This research identified the components of organizational resilience in hospitals amid crises and disasters. To accomplish this objective, a comprehensive review of both domestic and international databases was carried out. The literature review results revealed numerous elements crucial to comprehending the organizational resilience of hospitals in times of crises and disasters, among which the most significant are as follows: dimensions of vulnerability, preparedness, support management, responsiveness, and adaptability during crisis and post-crisis recovery. In the context of organizational resilience during emergencies and disasters, a hospital’s vulnerability pertains to its capacity and robustness in withstanding injuries and threats throughout the crisis. This facet of the hospital’s organizational resilience emphasizes pinpointing vulnerabilities and weak spots within the hospital’s structure, processes, resources, and equipment, as well as the steps required to bolster them against crises and disasters. The primary components of the vulnerability aspect in hospital resilience include the following items: pinpointing vulnerabilities, evaluating risks, implementing preventive strategies, preparing resources, and collaborating with other entities and organizations. The vulnerability aspect of hospital resilience underscores fortifying the weak and susceptible areas in the hospital’s structure and functioning to mitigate the impacts of crises and disasters on the institution. In supporting this dimension, Carrington et al. in their review article, regarded comprehending risk and disaster as the foremost priority and bolstering disaster risk governance as the secondary priority. Accordingly, a risk assessment should be conducted to ascertain the hospital’s susceptibility to particular disasters, and risk management strategies should be developed to enhance disaster resilience broadly [16]. Additionally, in qualitative research conducted at Ilam University of Medical Sciences, Bazyar et al. emphasized the indispensable role of risk information for accurate risk management about vulnerability [12]. Furthermore, in their article focused on outlining the components of organizational resilience in military hospitals, Zaboli et al. identified vulnerability and safety as one of the five primary dimensions of their model [42]. Within the framework of organizational resilience for hospitals during crises and disasters, preparedness alludes to the collection of actions and procedures that equip the hospital to confront crises and potential harm, ensuring the hospital’s consistent operation under both regular and critical circumstances. Key attributes and activities of preparedness within the hospital’s organizational resilience encompass the creation and execution of training programs, formulation and deployment of operational plans, provisioning of equipment and infrastructure, drills and critical exercises, communication and data dissemination, as well as evaluation and ongoing refinement. It is beneficial for these factors and activities to be executed in collaboration with various hospital teams, including managers, medical staff, and other affiliated institutions and organizations, to enhance the hospital’s organizational preparedness and resilience during crises and disasters. In support of this view, Bazyar et al. in their qualitative research at Ilam University of Medical Sciences note that even with the extensive negative repercussions disasters have across human, economic, social, and environmental facets, they are persistently perceived as opportunities and drivers for advancement. By capitalizing on limited chances, an individual can prepare for the present crisis but also attain a degree of preparedness for potential future disasters [12]. Moreover, in their study on Indonesian hospitals, Sunindijo et al. assert that the hospital safety index serves as a valuable instrument for assessing hospital preparedness and resilience during emergencies and disasters and pinpointing areas requiring enhancement. Hospitals and governing bodies can utilize hospital safety index outcomes to prioritize and enact essential measures to enhance hospital efficiency [31]. In their study evaluating eight hospitals in southwest Iran, Shir Ali et al. point out that the preparedness level of these institutions is subpar. Notable shortcomings included the absence of a current, written preparedness plan, a lack of an in-house disaster response team, insufficient training, an absence of disaster drills to hone staff skills and assess their capacities, underdeveloped communication infrastructures, and a dearth of mutual assistance agreements or memorandums of understanding. Additionally, the minimal to nonexistent budget allocation for procuring vehicles and equipment was identified as one of the weak links in the hospitals’ preparedness [27]. In the context of hospital resilience, support management pertains to the administration and utilization of supportive resources and equipment, like communication systems, maintenance and repair mechanisms, medical devices, etc. to sustain and enhance the hospital’s functionality during critical situations and amid natural or man-made disasters. This aspect encompasses the planning, design, and execution of support strategies, upkeep of equipment, enhancement of communication systems, and collaboration with other hospital departments during emergencies. This facet is crucial in upholding and augmenting the hospital’s resilience against potential risks and threats. In supporting this perspective, El-Sayed et al. highlighted in a case study detailing a Beirut hospital’s response to a mass casualty incident (car bomb explosion) event, how the surgery department, the blood bank, and the radiology department dispatched their staff to assist in coordinating the urgent needs arising from the sudden influx of patients to the emergency room [20]. There was a slight delay in deploying equipment, medicines, and supplies to the emergency room. Personnel from other departments who arrived to aid the emergency section noted challenges in accessing crucial equipment during the early response stage. A gap in the system was identified as unfamiliarity with the existing stockpiles. Drug carts were strategically positioned within the emergency department. Media served as the primary informant regarding the extent of damage from the crisis. Direct lines of communication were set up with responding EMS entities to guarantee real-time updates and feedback concerning patient movement and casualty allocation. Tasks such as managing fatalities, replenishing vital equipment, and refilling emergency medications were executed [20]. Within the framework of hospital organizational resilience, the aspect of response and adaptability during a crisis pertains to the collection of actions and strategies that enable the hospital to promptly and efficiently address immediate needs and challenges during crises and disasters. This facet of a hospital’s organizational resilience underscores its capacity to modify and adapt its operations under the unique and pressing circumstances presented by a crisis. Essential components of response and adaptability within hospital organizational resilience include organizational framework, crisis handling, communication and data dissemination, workforce, equipment and materials, and collaboration with other entities and organizations. Based on these components, the aspect of response and adaptability within hospital organizational resilience signifies equipping the hospital to tackle conditions posed by a crisis. Supporting this perspective, Zhong et al., in a study encompassing 41 tertiary hospitals in Shandong Province, China, assert that the capacity to address medical emergencies—encompassing emergency services and augmented capabilities (spanning on-site rescue, in-hospital care, and surge capacity)—stands as a pivotal resilience factor for a hospital [1]. Also, Blanchet et al. examine the resilience of a health system and state that the health system helps to coordinate employees in times of crisis or shock and to create bridges between different groups within this system and beyond. The capacity to anticipate and deal with uncertainties and unplanned events of resilience can be understood in terms of the adaptability of health systems. Adaptability is the capacity of actors of a system to respond to stresses and shocks [15]. Additionally, Sunindijo et al., in their study on Indonesian hospitals, highlight that the capacity to increase usable space during mass casualty events, sufficient logistical equipment in major catastrophes, procedures for transferring and admitting patients during emergencies and disasters, a strategy for infection prevention and control, and protocols for managing deceased bodies are among the critical response elements of a hospital during a crisis [31]. In the context of hospital organizational resilience, post-crisis recovery denotes a phase in the resilience journey where, following a crisis or disaster, the hospital endeavors to revert to its regular state and restore its standard operations. This facet of hospital organizational resilience focuses on managing the processes of recuperation and reinvigorating activities, mending and rebuilding infrastructure, and securing the necessary resources to sustain operations. Central components of post-crisis recovery within the hospital’s organizational resilience include repair and rebuilding, operational resurgence, restoration of communication and information, ensuring security, organizational adaptability (the institution’s capability to adjust to post-crisis changes and new conditions), and the organization’s competence in handling unforeseen and unexpected situations. In the context of a hospital’s organizational resilience, post-crisis recovery underscores managing activities, resources, and infrastructure vital for returning the hospital to its regular state and ensuring the continued delivery of services to patients in a secure and consistent environment. In supporting this perspective, Carrington et al., in their review, emphasize enhancing disaster preparedness for an efficient response and highlight “better reconstruction” during recovery, rehabilitation, and reconstruction phases as the fourth priority of their research. This priority aligns with the Sendai framework for disaster risk reduction 2015-2030, a focus that wasn’t present in earlier studies [16]. Furthermore, Fallah Aliabadi et al., in their review, indicate that the derived metrics about recovery and response are seen as the organization’s velocity. This measure of resilience mirrors the hospital system’s ability to address priorities to reinstate functionality and avert future interruptions [43]. Additionally, in their research, Shir Ali et al. Highlight that the examined hospitals exhibit unsatisfactory conditions concerning post-crisis recovery. Analyzing the results revealed deficiencies, including the absence of a disaster recovery plan and recovery management. This might be attributed to the management system’s oversight of the recovery phase, possibly due to a prevailing emphasis on negating or diminishing the recovery necessity [27]. Overall, hospital resilience is crucial during crises and both natural and man-made disasters. The elements highlighted in this discussion can serve as potent strategies for bolstering hospital resilience. Consequently, these factors ought to be integral to health and welfare policymaking.
Conclusion
Within the healthcare system, the hospital stands as the foremost and most intricate entity for delivering medical services. It plays a pivotal role in lowering mortality rates and attending to the injured due to its provision of essential health and life-saving services. Consequently, the resilience of hospitals holds significant importance during crises, whether natural or human-induced. Based on the studies and research presented in this article, various pivotal elements influencing the organizational resilience of hospitals in times of crises and disasters have been pinpointed. These elements aid in fortifying and enhancing the preparedness of hospitals to adeptly navigate crises and disasters. This study structured these components into specific dimensions, namely vulnerability, preparedness, support management, response and adaptability during a crisis, and post-crisis recovery. During our exploration, post-crisis recovery emerged as a particularly vital facet of a hospital’s organizational resilience in crises and disasters. Additionally, various factors, such as initial planning, equipment and facility provisioning, staff training, communication, and resource management are crucial in bolstering the resilience of hospitals during both natural and human-induced disasters. Given these factors, policymakers and administrators should prioritize these components, incorporating them as fundamental elements of health and therapeutic strategies. Furthermore, enhancing the resilience of hospitals, being a consistent and ongoing process, necessitates collaboration and coordination among the government, private sector, and the broader community. Consequently, emphasizing the resilience of hospitals, a pivotal matter in healthcare will bolster confidence and public faith in the nation’s healthcare infrastructure.
Study limitations
Restriction of access to certain databases and the unavailability of full-text articles hindered the research. The organizational frameworks of medical centers vary across countries, leading to significant variations in the analysis of results.
Ethical Considerations
The current study was registered with the Ethics Committee of Qazvin University of Medical Sciences (Code: IR.QUMS.REC.1400.438).
Funding
This study was an integral component of the final project for the master’s thesis of Fatemeh Seyghalani Talab, approved by the Faculty of Health, Qazvin University of Medical Sciences.
Authors' contributions
Study design: Omid Khosravizadeh; Research: Fatemeh Seyghalani Talab; Data analysis: Bahman Ahadinezhad; Writing and final approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors are grateful to the administrators and staff of Qazvin University of Medical Sciences.
References
Disasters can disturb a wide array of infrastructures and facilities, ranging from hospitals to educational institutions, transportation networks, and emergency services. Meanwhile, hospitals play a crucial role in critical circumstances as they mitigate the impact of such situations and decrease fatalities resulting from them [1]. As a result, efficient disaster management within hospitals is considered an essential approach to ensuring uninterrupted healthcare services amid crises, even when hospitals are directly impacted by such situations [2]. To manage crises effectively, a systematic procedure is required for executing organizational choices, enacting policies, devising solutions, and harnessing societal capabilities. This process mitigates the impact and detrimental outcomes of disasters. Among the pivotal phases of health-related crisis management is the capacity of the healthcare and treatment system to foster resilience, ensuring the provision of health and treatment services [3]. Conversely, hospital resilience is characterized as the hospitals’ capability to withstand, assimilate, and react to the impacts of critical circumstances, while upholding the continuity of vital health services and subsequently restoring the original state or adjusting to novel conditions. This description alludes to a holistic outlook on the hospital’s capacity to address urgent scenarios, encompassing inherent robustness (the capacity to endure and assimilate crises) and adaptable versatility (approaches to sustain the provision of crucial health services and adjust to forthcoming crises) [4]. Hence, assessing and communicating the status of hospitals and clinics constitutes the initial stride in readying them for emergencies and disasters. This evaluation encompasses identifying hazards, assessing both structural and non-structural vulnerabilities, evaluating functional preparedness, and considering diverse human and logistical capabilities as the primary measures to enhance hospitals’ preparedness to face accidents and crises [5, 6]. Regularly performing this assessment can furnish the necessary information and steps to enhance the effectiveness of health and treatment systems. To achieve this goal, it is essential to have a clear understanding of existing capacities, enabling the formulation of plans and actions that leverage these capacities to enhance the system’s resilience [6, 7]. As indicated earlier, the necessity to secure the uninterrupted provision of services within organizations has attained its pinnacle significance, given that it is of utmost importance to ascertain the capacity of organizations to handle emergencies and disasters [6]. Possessing a proficient initiative in appraising resilience management holds a pivotal position in ensuring the triumph of the continuity of organizational operations. Past instances have demonstrated that entities lacking a consistent and systematic strategy for overseeing hazardous processes have encountered numerous emergencies and disasters, leading to human casualties, financial setbacks, and environmental detriment [3]. Given that disturbances and discrepancies within hospitals can result in irreparable harm and losses, it becomes highly crucial to motivate researchers and decision-makers to develop remedies aimed at enhancing resilience within health and treatment facilities [8]. Considering the significance of hospitals’ continuous provision of services and the value of assessment, monitoring, and planning to enhance hospitals’ resilience against accidents, along with a review of relevant studies, the present research investigates the constituents of organizational resilience within hospitals during times of emergency and disasters.
Materials and Methods
Study design
This investigation was carried out as a comprehensive review aimed at identifying the organizational resilience elements of hospitals during crisis and disaster occurrences in 2022.
Research question and framework
The current study addresses this question “What constitutes organizational resilience elements within hospitals during emergencies and disasters?” It is structured around a multi-part conceptual framework, as depicted in Figure 1.
Search strategy
The data was collected by consulting PubMed, Web of Science, Magiran, SID, and Irandoc databases from 2012 to 2022. To identify and cover more articles, a manual search of some key authoritative journals was also done. The keywords included “sustainability”, “resilience”, “strategy”, “medical centers”, “healthcare”, “hospital”, “organizational resilience”, “crisis”, “disaster”, “emergency”, “health services”, “medical services”, and “health system” (Table 1).

“AND”, “or”, and “not” operators were used to combine or limit the search results.
Inclusion and exclusion criteria
To select the articles pertinent to the research domain, the criteria for inclusion comprised the following items: 1) Studies carried out within the last decade in the realm of hospital organizational resilience; 2) All types of descriptive, analytical, and cross-sectional studies that utilize various methodologies; and 3) Studies written only in the English and Persian languages. Meanwhile, the exclusion criteria were studies that were done in other service areas and studies that were not accessible.
Screening and selection of studies
Articles featuring keywords within their titles and abstracts were picked, followed by the identification and elimination of duplicate articles from the review procedure. Subsequently, the abstracts were assessed, followed by a thorough examination of the complete texts of the articles. Studies that aligned poorly with the study objectives and incorporated exclusion criteria were recognized and excluded. Ultimately, a compilation of titles for all the articles sourced from the database was generated. To establish the most fitting inventory, a screening process was conducted, during which irrelevant articles were eliminated. Lastly, the chosen articles were incorporated into the study. The selected articles were meticulously examined and assessed. The categorization and arrangement of titles, along with the detection and elimination of duplicate entries, were all facilitated through resource management software (EndNote X6).
Quality assessment and data extraction
Following the search, the gathered articles underwent evaluation by the researchers utilizing the strengthening of the reporting of observational studies in the epidemiology checklist. Articles of high quality were chosen by this assessment. This checklist stands as one of the prime instruments employed to assess the quality of observational articles. This checklist comprises 22 criteria spanning sections such as title, introduction, methodology, results, discussion, and conclusion. Articles failing to meet over 50% of the checklist criteria were excluded. Data extraction was carried out after the quality assessment. Necessary data, including author and year of publication, study location, study title, target population, study type, methodology, and key findings were extracted and succinctly summarized.
Category of results
The elements extracted in this study were organized into distinct dimensions. During this analysis, the re searchers individually classified the extracted components from the studies into various dimensions. Subsequently, the formulated dimensions and components were juxtaposed, and the researchers harmonized and presented a unanimous categorization. Then, the established dimensions and components were juxtaposed, and the researchers collated and presented a mutually agreed-upon singular classification.
Results
Several studies were conducted at different stages of the research, and 2442 studies were identified from the database search. An initial 701 articles were excluded due to their lack of titles pertinent to the study objectives, redundancy, and unavailability of the full article text. In the subsequent phase, after reviewing the abstracts of the articles, a total of 1659 articles were eliminated from consideration due to their lack of results relevant to our objectives. In the third stage, by studying the full text of the remaining articles, 62 articles were excluded due to the existence of similar Persian and English versions, being unrelated to the topic, and not having the necessary quality. Ultimately, a total of 20 articles that exhibited the closest alignment to the research topic were incorporated into the final analysis (Figure 2). The research examined a total of 20 final articles, consisting of 15 foreign studies and 5 domestic studies. Table 2 provides a summary of the reviewed studies, presenting various information, such as the article title, authors’ names, year of publication, study purpose and population, and the study type and methodology.
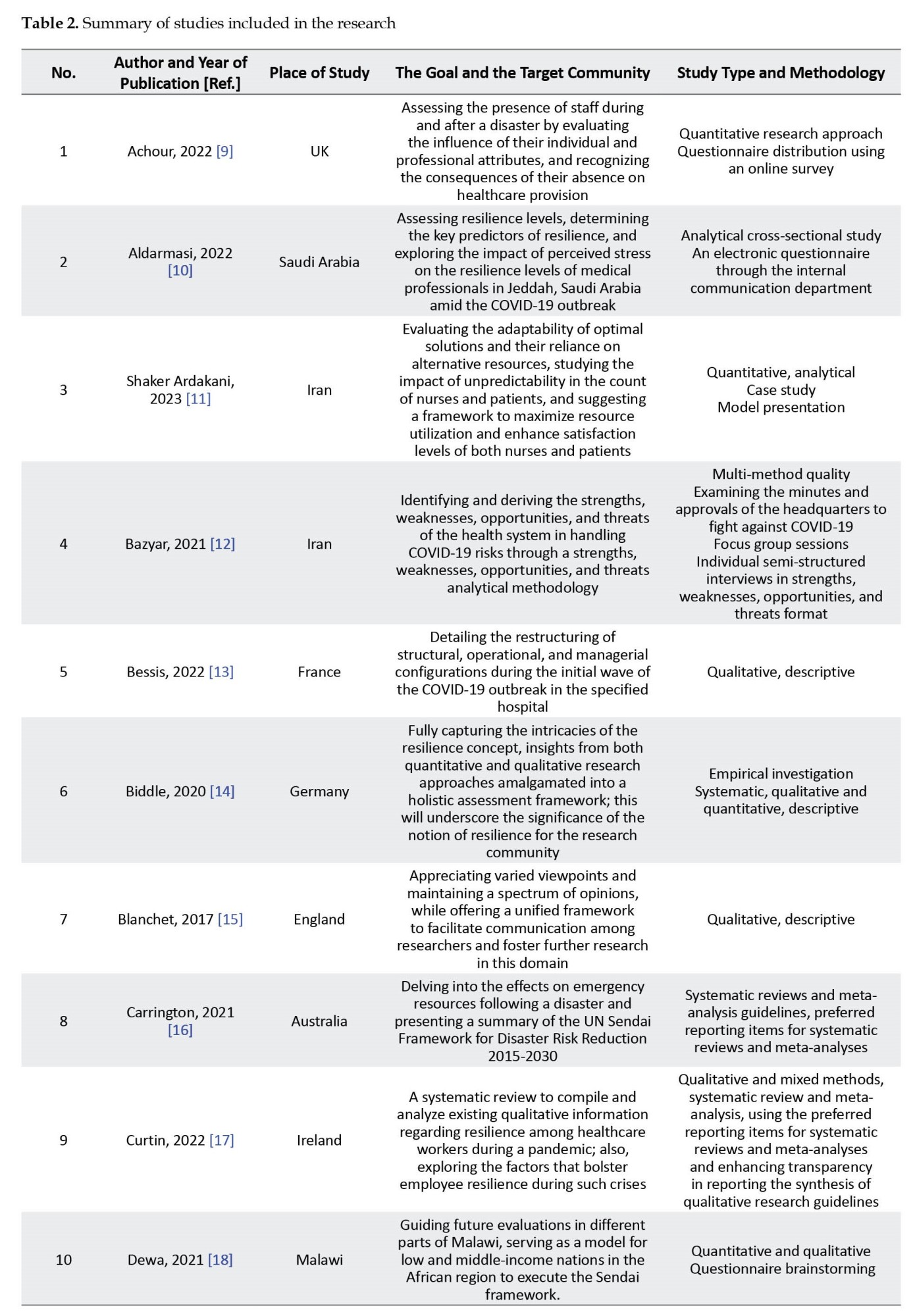

After closely analyzing 20 selected articles, the components of organizational resilience for hospitals during crises and disasters were categorized into five dimensions as follows: Vulnerability, preparedness, support management, responsiveness and adaptability during an emergency, and recovery after the emergency. The vulnerability dimension encompasses the recognized weaknesses that a set possesses about certain risks. A hospital’s vulnerability is influenced by its preparedness level. For instance, if a hospital is highly prepared for an earthquake, its susceptibility to it diminishes correspondingly. The preparedness dimension pertains to the idea of anticipating issues in human performance and indicates how the organization responds to significant incidents and crises, along with executing strategies in this area. It oversees the management of assistance, provision of resources, and other essential items needed to attain the operational objectives set by the incident command. Additionally, during a crisis, the response and adaptability phase is when the plan to address incidents is genuinely activated, to preserve human lives, offering first aid, mitigating and repairing system damages, and delivering necessary services to the victims. In essence, adaptability during a crisis means accelerating improvements. This is a crucial function of the hospital. Lastly, post-crisis recovery encompasses all actions undertaken to bring the hospital back to its pre-incident state. This procedure involves rebuilding existing buildings and infrastructures, restoring sub-structures, resettling the community, and offering essential mental health services to those who survived. The elements identified in the articles have been categorized and presented according to pre-established dimensions (Table 3).


Discussion
This research identified the components of organizational resilience in hospitals amid crises and disasters. To accomplish this objective, a comprehensive review of both domestic and international databases was carried out. The literature review results revealed numerous elements crucial to comprehending the organizational resilience of hospitals in times of crises and disasters, among which the most significant are as follows: dimensions of vulnerability, preparedness, support management, responsiveness, and adaptability during crisis and post-crisis recovery. In the context of organizational resilience during emergencies and disasters, a hospital’s vulnerability pertains to its capacity and robustness in withstanding injuries and threats throughout the crisis. This facet of the hospital’s organizational resilience emphasizes pinpointing vulnerabilities and weak spots within the hospital’s structure, processes, resources, and equipment, as well as the steps required to bolster them against crises and disasters. The primary components of the vulnerability aspect in hospital resilience include the following items: pinpointing vulnerabilities, evaluating risks, implementing preventive strategies, preparing resources, and collaborating with other entities and organizations. The vulnerability aspect of hospital resilience underscores fortifying the weak and susceptible areas in the hospital’s structure and functioning to mitigate the impacts of crises and disasters on the institution. In supporting this dimension, Carrington et al. in their review article, regarded comprehending risk and disaster as the foremost priority and bolstering disaster risk governance as the secondary priority. Accordingly, a risk assessment should be conducted to ascertain the hospital’s susceptibility to particular disasters, and risk management strategies should be developed to enhance disaster resilience broadly [16]. Additionally, in qualitative research conducted at Ilam University of Medical Sciences, Bazyar et al. emphasized the indispensable role of risk information for accurate risk management about vulnerability [12]. Furthermore, in their article focused on outlining the components of organizational resilience in military hospitals, Zaboli et al. identified vulnerability and safety as one of the five primary dimensions of their model [42]. Within the framework of organizational resilience for hospitals during crises and disasters, preparedness alludes to the collection of actions and procedures that equip the hospital to confront crises and potential harm, ensuring the hospital’s consistent operation under both regular and critical circumstances. Key attributes and activities of preparedness within the hospital’s organizational resilience encompass the creation and execution of training programs, formulation and deployment of operational plans, provisioning of equipment and infrastructure, drills and critical exercises, communication and data dissemination, as well as evaluation and ongoing refinement. It is beneficial for these factors and activities to be executed in collaboration with various hospital teams, including managers, medical staff, and other affiliated institutions and organizations, to enhance the hospital’s organizational preparedness and resilience during crises and disasters. In support of this view, Bazyar et al. in their qualitative research at Ilam University of Medical Sciences note that even with the extensive negative repercussions disasters have across human, economic, social, and environmental facets, they are persistently perceived as opportunities and drivers for advancement. By capitalizing on limited chances, an individual can prepare for the present crisis but also attain a degree of preparedness for potential future disasters [12]. Moreover, in their study on Indonesian hospitals, Sunindijo et al. assert that the hospital safety index serves as a valuable instrument for assessing hospital preparedness and resilience during emergencies and disasters and pinpointing areas requiring enhancement. Hospitals and governing bodies can utilize hospital safety index outcomes to prioritize and enact essential measures to enhance hospital efficiency [31]. In their study evaluating eight hospitals in southwest Iran, Shir Ali et al. point out that the preparedness level of these institutions is subpar. Notable shortcomings included the absence of a current, written preparedness plan, a lack of an in-house disaster response team, insufficient training, an absence of disaster drills to hone staff skills and assess their capacities, underdeveloped communication infrastructures, and a dearth of mutual assistance agreements or memorandums of understanding. Additionally, the minimal to nonexistent budget allocation for procuring vehicles and equipment was identified as one of the weak links in the hospitals’ preparedness [27]. In the context of hospital resilience, support management pertains to the administration and utilization of supportive resources and equipment, like communication systems, maintenance and repair mechanisms, medical devices, etc. to sustain and enhance the hospital’s functionality during critical situations and amid natural or man-made disasters. This aspect encompasses the planning, design, and execution of support strategies, upkeep of equipment, enhancement of communication systems, and collaboration with other hospital departments during emergencies. This facet is crucial in upholding and augmenting the hospital’s resilience against potential risks and threats. In supporting this perspective, El-Sayed et al. highlighted in a case study detailing a Beirut hospital’s response to a mass casualty incident (car bomb explosion) event, how the surgery department, the blood bank, and the radiology department dispatched their staff to assist in coordinating the urgent needs arising from the sudden influx of patients to the emergency room [20]. There was a slight delay in deploying equipment, medicines, and supplies to the emergency room. Personnel from other departments who arrived to aid the emergency section noted challenges in accessing crucial equipment during the early response stage. A gap in the system was identified as unfamiliarity with the existing stockpiles. Drug carts were strategically positioned within the emergency department. Media served as the primary informant regarding the extent of damage from the crisis. Direct lines of communication were set up with responding EMS entities to guarantee real-time updates and feedback concerning patient movement and casualty allocation. Tasks such as managing fatalities, replenishing vital equipment, and refilling emergency medications were executed [20]. Within the framework of hospital organizational resilience, the aspect of response and adaptability during a crisis pertains to the collection of actions and strategies that enable the hospital to promptly and efficiently address immediate needs and challenges during crises and disasters. This facet of a hospital’s organizational resilience underscores its capacity to modify and adapt its operations under the unique and pressing circumstances presented by a crisis. Essential components of response and adaptability within hospital organizational resilience include organizational framework, crisis handling, communication and data dissemination, workforce, equipment and materials, and collaboration with other entities and organizations. Based on these components, the aspect of response and adaptability within hospital organizational resilience signifies equipping the hospital to tackle conditions posed by a crisis. Supporting this perspective, Zhong et al., in a study encompassing 41 tertiary hospitals in Shandong Province, China, assert that the capacity to address medical emergencies—encompassing emergency services and augmented capabilities (spanning on-site rescue, in-hospital care, and surge capacity)—stands as a pivotal resilience factor for a hospital [1]. Also, Blanchet et al. examine the resilience of a health system and state that the health system helps to coordinate employees in times of crisis or shock and to create bridges between different groups within this system and beyond. The capacity to anticipate and deal with uncertainties and unplanned events of resilience can be understood in terms of the adaptability of health systems. Adaptability is the capacity of actors of a system to respond to stresses and shocks [15]. Additionally, Sunindijo et al., in their study on Indonesian hospitals, highlight that the capacity to increase usable space during mass casualty events, sufficient logistical equipment in major catastrophes, procedures for transferring and admitting patients during emergencies and disasters, a strategy for infection prevention and control, and protocols for managing deceased bodies are among the critical response elements of a hospital during a crisis [31]. In the context of hospital organizational resilience, post-crisis recovery denotes a phase in the resilience journey where, following a crisis or disaster, the hospital endeavors to revert to its regular state and restore its standard operations. This facet of hospital organizational resilience focuses on managing the processes of recuperation and reinvigorating activities, mending and rebuilding infrastructure, and securing the necessary resources to sustain operations. Central components of post-crisis recovery within the hospital’s organizational resilience include repair and rebuilding, operational resurgence, restoration of communication and information, ensuring security, organizational adaptability (the institution’s capability to adjust to post-crisis changes and new conditions), and the organization’s competence in handling unforeseen and unexpected situations. In the context of a hospital’s organizational resilience, post-crisis recovery underscores managing activities, resources, and infrastructure vital for returning the hospital to its regular state and ensuring the continued delivery of services to patients in a secure and consistent environment. In supporting this perspective, Carrington et al., in their review, emphasize enhancing disaster preparedness for an efficient response and highlight “better reconstruction” during recovery, rehabilitation, and reconstruction phases as the fourth priority of their research. This priority aligns with the Sendai framework for disaster risk reduction 2015-2030, a focus that wasn’t present in earlier studies [16]. Furthermore, Fallah Aliabadi et al., in their review, indicate that the derived metrics about recovery and response are seen as the organization’s velocity. This measure of resilience mirrors the hospital system’s ability to address priorities to reinstate functionality and avert future interruptions [43]. Additionally, in their research, Shir Ali et al. Highlight that the examined hospitals exhibit unsatisfactory conditions concerning post-crisis recovery. Analyzing the results revealed deficiencies, including the absence of a disaster recovery plan and recovery management. This might be attributed to the management system’s oversight of the recovery phase, possibly due to a prevailing emphasis on negating or diminishing the recovery necessity [27]. Overall, hospital resilience is crucial during crises and both natural and man-made disasters. The elements highlighted in this discussion can serve as potent strategies for bolstering hospital resilience. Consequently, these factors ought to be integral to health and welfare policymaking.
Conclusion
Within the healthcare system, the hospital stands as the foremost and most intricate entity for delivering medical services. It plays a pivotal role in lowering mortality rates and attending to the injured due to its provision of essential health and life-saving services. Consequently, the resilience of hospitals holds significant importance during crises, whether natural or human-induced. Based on the studies and research presented in this article, various pivotal elements influencing the organizational resilience of hospitals in times of crises and disasters have been pinpointed. These elements aid in fortifying and enhancing the preparedness of hospitals to adeptly navigate crises and disasters. This study structured these components into specific dimensions, namely vulnerability, preparedness, support management, response and adaptability during a crisis, and post-crisis recovery. During our exploration, post-crisis recovery emerged as a particularly vital facet of a hospital’s organizational resilience in crises and disasters. Additionally, various factors, such as initial planning, equipment and facility provisioning, staff training, communication, and resource management are crucial in bolstering the resilience of hospitals during both natural and human-induced disasters. Given these factors, policymakers and administrators should prioritize these components, incorporating them as fundamental elements of health and therapeutic strategies. Furthermore, enhancing the resilience of hospitals, being a consistent and ongoing process, necessitates collaboration and coordination among the government, private sector, and the broader community. Consequently, emphasizing the resilience of hospitals, a pivotal matter in healthcare will bolster confidence and public faith in the nation’s healthcare infrastructure.
Study limitations
Restriction of access to certain databases and the unavailability of full-text articles hindered the research. The organizational frameworks of medical centers vary across countries, leading to significant variations in the analysis of results.
Ethical Considerations
The current study was registered with the Ethics Committee of Qazvin University of Medical Sciences (Code: IR.QUMS.REC.1400.438).
Funding
This study was an integral component of the final project for the master’s thesis of Fatemeh Seyghalani Talab, approved by the Faculty of Health, Qazvin University of Medical Sciences.
Authors' contributions
Study design: Omid Khosravizadeh; Research: Fatemeh Seyghalani Talab; Data analysis: Bahman Ahadinezhad; Writing and final approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors are grateful to the administrators and staff of Qazvin University of Medical Sciences.
References
- Zhong S, Clark M, Hou XY, Zang Y, FitzGerald G. Validation of a framework for measuring hospital disaster resilience using factor analysis. International Journal of Environmental Research and Public Health. 2014; 11(6):6335-53. [DOI:10.3390/ijerph110606335] [PMID]
- Sauer LM, McCarthy ML, Knebel A, Brewster P. Major influences on hospital emergency management and disaster preparedness. Disaster Medicine and Public Health Preparedness. 2009; 3(2 Suppl):S68-73. [DOI:10.1097/DMP.0b013e31819ef060] [PMID]
- Ahesteh H, Rouhollahei M, Jalali Farahani A. Assessment the resilience of the healthcare network in accidents and chemical crises. Journal of Military Medicine. 2020; 22(7):747-59. [DOI:10.30491/JMM.22.7.9]
- Zhong S, Clark M, Hou XY, Zang YL, Fitzgerald G. Development of hospital disaster resilience: Conceptual framework and potential measurement. Emergency Medicine Journal. 2014; 31(11):930-8. [DOI:10.1136/emermed-2012-202282] [PMID]
- Ardalan A, Kandi M, Talebian MT, Khankeh H, Masoumi G, Mohammadi R, et al. Hospitals safety from disasters in IR iran: The results from assessment of 224 hospitals. PLoS Currents. 2014; 6:ecurrents.dis.8297b528bd45975bc6291804747ee5db. [PMID]
- Svata V. System view of business continuity management. Journal of Systems Integration. 2013; 4(2):19-35. [Link]
- Azadeh A, Fam IM, Nouri J, Azadeh MA. Integrated health, safety, environment and ergonomics management system (HSEE-MS): An efficient substitution for conventional HSE-MS. Journal of Scientific & Industrial Research. 2008; 67:403-11. [Link]
- Aiello A, Khayeri MY, Raja S, Peladeau N, Romano D, Leszcz M, et al. Resilience training for hospital workers in anticipation of an influenza pandemic. Journal of Continuing Education in the Health Professions. 2011; 31(1):15-20. [DOI:10.1002/chp.20096] [PMID]
- Achour N, Elhaj H, Ali A. Hospital resilience to extreme events: A staff capability of attendance perspective. International Journal of Disaster Risk Reduction. 2022; 72:102851. [DOI:10.1016/j.ijdrr.2022.102851]
- Aldarmasi MA. Factors associated with resilience among healthcare professionals during the COVID-19 pandemic: A cross-sectional study. Cureus. 2022; 14(5):e25106. [DOI:10.7759/cureus.25106] [PMID]
- Shaker Ardakani E, Gilani Larimi N, Oveysi Nejad M, Madani Hosseini M, Zargoush M. A resilient, robust transformation of healthcare systems to cope with COVID-19 through alternative resources. Omega. 2023; 114:102750. [DOI:10.1016/j.omega.2022.102750] [PMID]
- Bazyar J, Alimoradi S, Seydi M, Pourvakhshoori N, Sadeghifar J. Coronavirus disease-2019 risk management using strengths, weaknesses, opportunities, threats analysis approach in the health system: A qualitative multimethod study. Journal of Education and Health Promotion. 2021; 10:453. [PMID]
- Bessis S, Dinh A, Gautier S, Davido B, Levy J, Lawrence C, et al. A restructured hospital into a one-building organization for COVID-19 patients: A resilient and effective response to the pandemic. Frontiers in Public Health. 2022; 10:709848. [DOI:10.3389/fpubh.2022.709848] [PMID]
- Biddle L, Wahedi K, Bozorgmehr K. Health system resilience: A literature review of empirical research. Health Policy and Planning. 2020; 35(8):1084-109. [DOI:10.1093/heapol/czaa032] [PMID]
- Blanchet K, Nam SL, Ramalingam B, Pozo-Martin F. Governance and capacity to manage resilience of health systems: Towards a new conceptual framework. International Journal of Health Policy and Management. 2017; 6(8):431-5. [DOI:10.15171/ijhpm.2017.36] [PMID]
- Carrington MA, Ranse J, Hammad K. The impact of disasters on emergency department resources: Review against the Sendai framework for disaster risk reduction 2015-2030. Australasian Emergency Care. 2021; 24(1):55-60. [DOI:10.1016/j.auec.2020.09.003] [PMID]
- Curtin M, Richards HL, Fortune DG. Resilience among health care workers while working during a pandemic: A systematic review and meta synthesis of qualitative studies. Clinical Psychology Review. 2022; 24(1):55-60. [DOI:10.1016/j.cpr.2022.102173] [PMID]
- Dewa O, Makoka D, Ayo-Yusuf OA. Assessing capacity and implementation status of the disaster risk management strategy for health and community disaster resilience in Malawi. International Journal of Disaster Risk Science. 2021; 12:673-88. [DOI:10.1007/s13753-021-00369-z]
- Donelli CC, Fanelli S, Zangrandi A, Elefanti M. Disruptive crisis management: Lessons from managing a hospital during the COVID-19 pandemic. Management Decision. 2022; 60(13):66-91. [DOI:10.1108/MD-02-2021-0279]
- El Sayed M, Chami AF, Hitti E. Developing a hospital disaster preparedness plan for mass casualty incidents: Lessons learned from the downtown beirut bombing. Disaster Medicine and Public Health Preparedness. 2018; 12(3):379-85. [DOI:10.1017/dmp.2017.83] [PMID]
- Fallah-Aliabadi S, Ostadtaghizadeh A, Ardalan A, Fatemi F, Khazai B, Mirjalili MR. Towards developing a model for the evaluation of hospital disaster resilience: A systematic review. BMC Health Services Research. 2020; 20(1):64. [DOI:10.1186/s12913-020-4915-2] [PMID]
- Ghanchi A. Insights into French emergency planning, response, and resilience procedures from a hospital managerial perspective following the Paris terrorist attacks of Friday, November 13, 2015. Disaster Medicine and Public Health Preparedness. 2016; 10(5):789-94. [DOI:10.1017/dmp.2016.21] [PMID]
- Hatefipour Z, Maghami Sharif Z, Farahani H, Aghebati A. Working in hospitals during a pandemic: Investigating the resilience among medical staff during COVID-19 outbreak through qualitative and quantitative research. Primary Health Care Research & Development. 2022; 23:e53. [DOI:10.1017/S1463423622000305] [PMID]
- Luke J, Franklin R, Aitken P, Dyson J. Safer hospital infrastructure assessments for socio-natural disaster-a scoping review. Prehospital and Disaster Medicine. 2021; 36(5):627-35. [DOI:10.1017/S1049023X21000650] [PMID]
- Marmo R, Pascale F, Diana L, Sicignano E, Polverino F. Lessons learnt for enhancing hospital resilience to pandemics: A qualitative analysis from Italy. International Journal of Disaster Risk Reduction. 2022; 81:103265. [DOI:10.1016/j.ijdrr.2022.103265] [PMID]
- Mohtady Ali H, Ranse J, Roiko A, Desha C. Investigating organizational learning and adaptations for improved disaster response towards “resilient hospitals:” An integrative literature review. Prehospital and Disaster Medicine. 2022; 37(5):665-73. [DOI:10.1017/S1049023X2200108X] [PMID]
- Shirali GA, Azadian Sh, Saki A. A new framework for assessing hospital crisis management based on resilience engineering approach. Work (Reading, Mass). 2016; 54(2):435-44. [DOI:10.3233/WOR-162329] [PMID]
- Stennett J, Hou R, Traverson L, Ridde V, Zinszer K, Chabrol F. Lessons learned from the resilience of Chinese hospitals to the COVID-19 pandemic: Scoping review. JMIRx med. 2022; 3(2):e31272. [DOI:10.2196/31272] [PMID]
- Achour N, Miyajima M, Pascale F, Price A DF. Hospital resilience to natural hazards: Classification and performance of utilities. Disaster Prevention and Management. 2014; 23(1):40-52. [DOI:10.1108/DPM-03-2013-0057]
- Capolongo S, Gola M, Brambilla A, Morganti A, Mosca EI, Barach P. COVID-19 and healthcare facilities: A decalogue of design strategies for resilient hospitals. Acta Bio Medica: Atenei Parmensis. 2020; 91(9-S):50-60. [DOI:10.23750/abm.v91i9-S.10117] [PMID]
- Sunindijo RY, Lestari F, Wijaya O. Hospital safety index: Assessing the readiness and resiliency of hospitals in Indonesia. Facilities. 2020; 38(1/2):39-51. [DOI:10.1108/F-12-2018-0149]
- Adini B, Cohen O, Eide AW, Nilsson S, Aharonson-Daniel L, Herrera IA. Striving to be resilient: What concepts, approaches and practices should be incorporated in resilience management guidelines? Technological Forecasting and Social Change. 2017; 121:39-49. [DOI:10.1016/j.techfore.2017.01.020]
- Aristodemou K, Buchhass L, Claringbould D. The COVID-19 crisis in the EU: The resilience of healthcare systems, government responses and their socio-economic effects. Eurasian Economic Review. 2021; 11:251-81. [DOI:10.1007/s40822-020-00162-1]
- Barbash IJ, Kahn JM. Fostering hospital resilience-lessons from COVID-19. JAMA. 2021; 326(8):693-4. [DOI:10.1001/jama.2021.12484] [PMID]
- Barasa E, Mbau R, Gilson L. What is resilience and how can it be nurtured? A systematic review of empirical literature on organizational resilience. International Journal of Health Policy and Management. 2018; 7(6):491-503. [DOI:10.15171/ijhpm.2018.06] [PMID]
- Chand AM, Loosemore M. A socio-ecological analysis of hospital resilience to extreme weather events. Construction Management and Economics. 2015; 33(11-12):907-20. [DOI:10.1080/01446193.2016.1165856]
- Alami H, Lehoux P, Fleet R, Fortin JP, Liu J, Attieh R, et al. How can health systems better prepare for the next pandemic? Lessons learned from the management of COVID-19 in Quebec (Canada). Frontiers in Public Health. 2021; 9:671833. [DOI:10.3389/fpubh.2021.671833] [PMID]
- Khosravizadeh O, Ahadinezhad B, Rafiei S, Kalhor R, Maleki A. COVID-19 crisis overshadowing the health workforces’ rights and resilience: a systematic review. International Journal of Human Rights in Healthcare. 2022; 15(5):477-88. [DOI: 10.1108/IJHRH-12-2021-0212]
- Adini B, Ohana A, Furman E, Ringel R, Golan Y, Fleshler E, et al. Learning lessons in emergency management: The 4th international conference on healthcare system preparedness and response to emergencies and disasters. Disaster and Military Medicine. 2016; 2:16. [DOI:10.1186/s40696-016-0026-3] [PMID]
- Aghapour AH, Yazdani M, Jolai F, Mojtahedi M. Capacity planning and reconfiguration for disaster-resilient health infrastructure. Journal of Building Engineering. 2019; 26:100853. [DOI:10.1016/j.jobe.2019.100853]
- Ammar W, Kdouh O, Hammoud R, Hamadeh R, Harb H, Ammar Z, et al. Health system resilience: Lebanon and the Syrian refugee crisis. Journal of Global Health. 2016; 6(2):020704. [DOI:10.7189/jogh.06.020704] [PMID]
- Zaboli R, Seyedin H, Nasiri A, Malmoon Z. Standardization and validation of organizational resilience tools in military hospitals. Journal of Military Medicine. 2022; 22(7):719-27. [DOI:10.30491/JMM.22.7.6]
- Fallah-Aliabadi S, Ostadtaghizadeh A, Fatemi F, Ardalan A, Rezaei E, Raadabadi M, et al. Hospital disaster resilience: Development of an assessment tool using expert panel and fuzzy analytical network process. International Journal of Disaster Resilience in the Built Environment. 2022; 13(5):554-67. [DOI:10.1108/IJDRBE-11-2020-0119]
Type of article: Review |
Subject:
General
Received: 2024/01/25 | Accepted: 2024/03/18 | Published: 2024/04/1
Received: 2024/01/25 | Accepted: 2024/03/18 | Published: 2024/04/1
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |